Losing Weight While Breastfeeding: How To Safely Shed Pounds Postpartum
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
If you are trying to lose weight while breastfeeding, you are in good company. Lactation uses energy and can support gentle postpartum weight loss, but you still need a plan. This guide shows you how to trim pounds safely without hurting your milk supply or your health.
You will learn simple steps that fit real life, plus what to avoid while you heal and feed your baby.
Key Takeaways
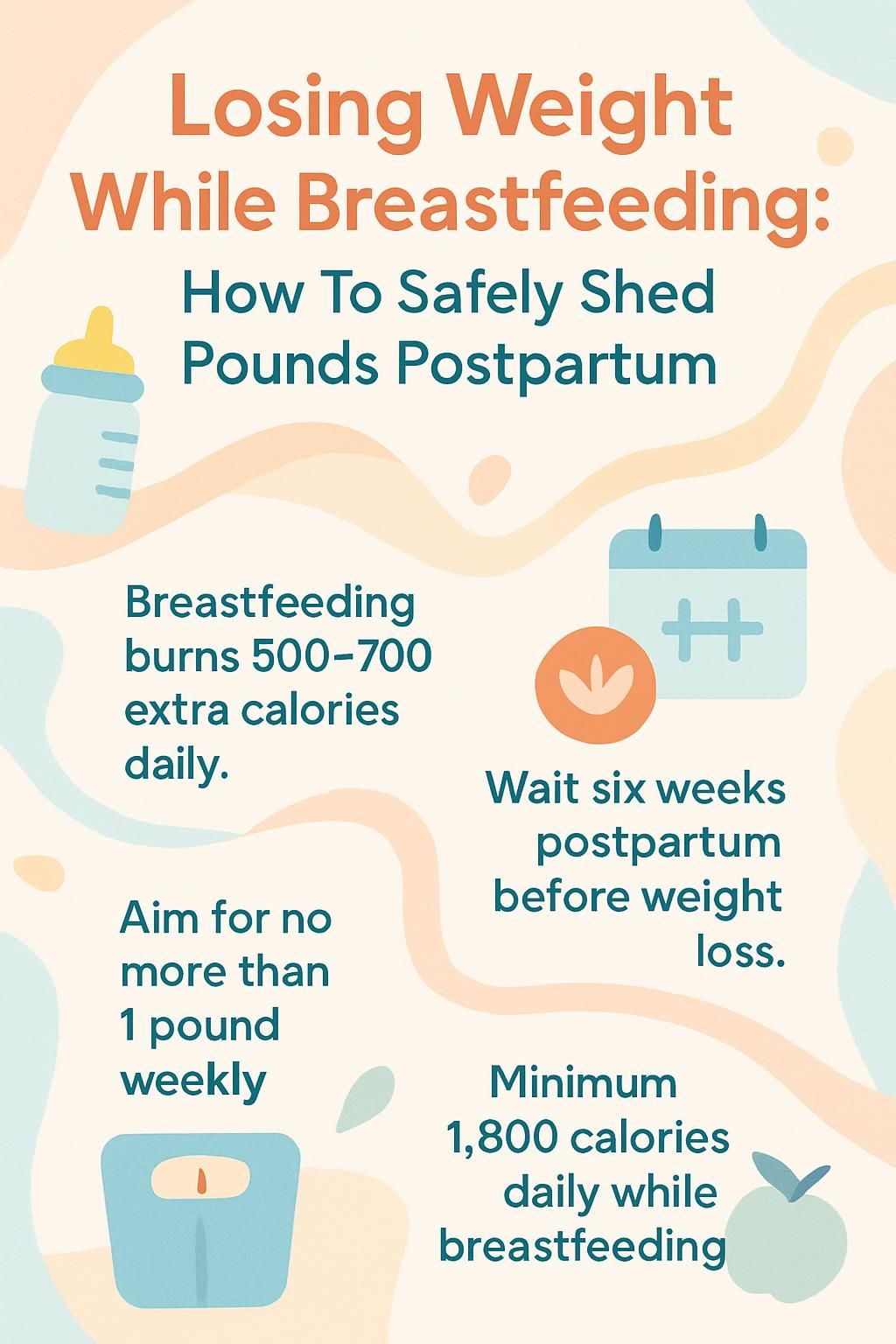
- Breastfeeding burns about 500 to 700 extra calories a day. Exclusive breastfeeding is linked to about 3.2 pounds more weight loss at 12 months postpartum (Dewey et al., 2001).
- Start weight loss efforts after your 6-week checkup. Aim for no more than about 1 pound per week to protect milk supply.
- Most breastfeeding moms need at least 1,800 calories daily. Very low calorie diets can sap energy, lower milk output, and slow infant growth.
- Trendy plans like intermittent fasting lack safety data for milk supply. Low-carb diets only work if balanced, varied, and calorie sufficient (Hart et al., 2022).
- Avoid weight loss drugs and supplements while nursing. Many products have unknown risks for infants; talk with your healthcare provider first (Campbell et al., 2024).
How Breastfeeding Affects Postpartum Weight Loss

Breastfeeding helps you burn extra calories, which can support slow and steady fat loss after pregnancy. Every body responds a bit differently because hormones, sleep, and activity level all matter.
How does breastfeeding burn calories?
Making breast milk takes energy. Most nursing parents use about 500 to 700 additional calories per day to produce and deliver milk. Your body uses food and stored fat to cover this demand, which can help weight come down over time.
Research, including Dewey et al., 2001, shows lactation raises daily energy use through metabolic and hormonal shifts. In studies, women who exclusively breastfed in the early months lost more weight by 12 months postpartum than those who did not.
Your body burns extra calories with every feeding session, and many moms compare that effort to a daily jog.
What factors affect weight loss after having a baby?
Several things shape postpartum weight change. Delivery type can affect recovery time. A cesarean birth often delays activity compared with a vaginal birth. Pre-pregnancy body mass index, pregnancy weight gain, and whether that gain matched medical guidelines also matter.
Dellapiana et al., 2024, highlight other influences like age, race or ethnicity, number of children, WIC use, support for breastfeeding, and whether the infant needed NICU care. Daily habits count too. More physical activity usually supports greater loss by 12 months.
Help from a clinician or a dietitian can make healthy changes easier, from planning balanced meals to building a walking routine. I found that gentle walks after an unplanned C-section helped me make slow progress without cutting calories too hard.
When Is the Best Time to Start Losing Weight After Birth?
Give your body time to heal before you focus on weight loss. Early recovery supports milk production, mood, and core strength.
Why is recovery time important before dieting?
Healing tissues, shifting hormones, and sleep debt make the first weeks demanding. Large calorie cuts before milk supply stabilizes, usually around 6 to 8 weeks, can stall recovery and drain energy needed for feeding and care.
The American Academy of Pediatrics and the Academy of Nutrition and Dietetics suggest waiting until your 6-week checkup to start intentional weight loss. Many people begin vigorous exercise around 6 to 12 weeks if cleared by a provider.
Give yourself grace; rest is part of recovery from childbirth.
Allowing time to heal supports a stable milk supply and a stronger return to activity.
What is the recommended timeline for postpartum weight loss?
Most experts recommend a gradual pace, about 1 pound, or 0.5 kg, per week. This approach protects your milk supply while moving you toward a healthy weight.
Wait until after the first six weeks to focus on losing weight. Exclusive breastfeeding often leads to greater loss at 12 months, with some studies noting about 3.2 pounds more compared with mixed or no breastfeeding.
Taking it slow can help you stay energized for feeds, diaper changes, and daily life with your baby.
Safe Weight Loss Guidelines for Breastfeeding Mothers
Safe weight loss keeps your milk supply steady and supports your mood, sleep, and recovery. A realistic target and enough food are key pillars.
How much weight loss is safe and gradual?
Aim to lose about 1 pound per week, and cap progress at about 4 pounds per month. The Academy of Nutrition and Dietetics notes that gradual loss of up to 1.5 pounds weekly usually does not lower milk production.
Rapid loss often comes from water or muscle, not fat. That pattern can lead to rebound gain later. If progress stalls, focus on small, steady changes instead of bigger cuts.
Consistent habits, like balanced meals and gentle activity, tend to work better than crash diets.
What are the calorie needs for breastfeeding moms?
Most breastfeeding moms need a minimum of 1,800 calories a day. Many need more, depending on size, activity, and supply. Exclusive breastfeeding uses about 500 extra calories daily compared with pre-pregnancy needs.
Choose nutrient-dense foods: colorful produce, whole grains, lean protein, and healthy fats. Eating regularly helps steady blood sugar and energy. Going below your calorie floor can reduce milk output and slow infant weight gain.
Skip very-low-calorie plans and weight loss medications unless a clinician approves them for you.
Dietary Changes to Support Milk Supply and Weight Loss
Food quality matters. A simple, balanced plan helps you lose weight slowly and keep your milk flowing.
Which nutrient-dense foods help postpartum weight loss?
Build most meals from the following options. They pack vitamins, minerals, protein, and fiber into each bite.
- Fruit: berries, oranges, apples, bananas. These add fiber and natural sweetness without added sugar.
- Vegetables: spinach, carrots, broccoli, sweet potatoes. Low in calories, high in micronutrients.
- Whole grains: brown rice, quinoa, oats, and 100 percent whole wheat bread for fiber and steady energy.
- Lean proteins: chicken, turkey, eggs, tofu, beans, and fish rich in omega-3s to support muscle repair and appetite control.
- Healthy fats: avocado, olives, nuts, and seeds to help with vitamin absorption and energy.
- Smart snacks: Greek yogurt with fruit or nuts for protein and calcium that support milk production.
- Fluids: water or herbal teas for hydration, which supports both supply and appetite regulation.
Prepping a few grab-and-go snacks, like cut fruit with yogurt, can reduce impulse eating and keep energy steady.
How important is hydration while breastfeeding?
Milk is mostly water, so your hydration status affects supply. Aim for at least 12 cups of fluid each day.
Keep a drink nearby at every feed. Choose water, seltzer, or unsweetened tea. Limit sugary beverages, which add calories without helpful nutrients.
Good hydration supports weight goals and helps prevent fatigue and headaches that can follow dehydration.
What foods should breastfeeding moms avoid or limit?
Some foods add calories without nutrition or carry safety concerns. Limiting these supports milk quality and weight goals.
- Highly processed items with trans fats, extra sodium, or many preservatives. Bake or broil instead of frying.
- Added sugars in soda, sweet teas, pastries, and candy. These are empty calories.
- Excess saturated fat from fatty meats, butter, and cream sauces. Use plant oils in moderation.
- Large servings of fruit juice. Whole fruit offers fiber and fullness. If you drink juice, keep it under 4 ounces per day.
- Restrictive plans that cut whole food groups, like very low-carb plans that drop produce or grains.
- Alcohol beyond one standard drink per day. Alcohol passes into milk.
- More than about 200 mg of caffeine daily, or roughly two small cups of coffee, if your baby seems sensitive.
- High-mercury fish: swordfish, king mackerel, shark, tilefish, per FDA guidance.
- Unpasteurized cheeses and deli meats, which can carry harmful bacteria.
Choosing whole foods most of the time helps you lose weight at a steady pace while keeping enough energy for long days and nights.
Exercising Safely While Breastfeeding
Movement helps you feel more like yourself again. With smart pacing and fuel, exercise and milk supply can coexist.
How to start with low-impact exercises postpartum?
Begin gently, then build. Low-impact movement supports healing while boosting mood and stamina.
- Start with easy walks in the first weeks. Work toward brisk walking 20 to 30 minutes most days.
- Add light stretching or postnatal yoga for flexibility and stress relief.
- Get medical clearance, especially after a cesarean or complications.
- Work toward at least 150 minutes of moderate aerobic activity per week. Short sessions count.
- Begin with 5 to 10 minutes a day, then increase time as energy returns.
- Wear supportive clothing and a well-fitted nursing bra to reduce discomfort.
- Pay attention to signals like pain, dizziness, or a clear drop in supply. Ease up if they appear.
- Delay high-impact workouts until your clinician says you are ready. Consistency matters more than intensity.
- Many parents find stroller walks build confidence and routine while keeping supply stable.
Low-impact exercise can support safe weight management without putting strain on healing tissues.
How to include strength training and cardio safely?
Cardio burns calories, and strength training protects muscle. Together, they support a healthy metabolism.
- Get clearance before vigorous exercise. Many people return to higher intensity at 6 to 12 weeks if healed.
- Use low-impact cardio first, such as walking or swimming, for 10 to 20 minutes a day.
- Add two short strength sessions weekly. Try bodyweight squats, wall push-ups, and gentle lunges.
- Increase intensity slowly as comfort and energy improve.
- Alternate cardio and strength days to protect muscle while you lose fat.
- Fuel workouts. Most breastfeeding parents need about 500 extra calories a day.
- Watch for warning signs like extreme fatigue or a clear drop in milk. Adjust if needed.
- Hydrate before, during, and after activity.
- Track how your body responds. Adjust time or weight based on recovery.
These steps help you combine nutrition changes with activity while safeguarding your milk supply.
What are tips for safe exercise during breastfeeding?
A few small tweaks can make workouts more comfortable and effective.
- Nurse or pump before exercise to reduce fullness and tenderness.
- Pick a supportive sports bra that limits bounce and chafing.
- Drink water before, during, and after workouts.
- Start with low-impact movement until about 6 to 12 weeks, or until you feel healed.
- Increase intensity gradually and watch for fatigue signals.
- Aim for about 150 minutes of moderate activity per week, or the amount your body tolerates.
- Avoid deep calorie cuts, especially below about 1,800 calories a day.
- Slow down if you notice reduced milk output or heavy exhaustion.
- Eat a nutrient-dense snack after workouts to refuel.
- Short sessions right after nursing often feel more comfortable.
Evidence suggests that exercise does not reduce milk volume or change taste when you stay hydrated and well nourished (Lauwers and Swisher, Campbell et al.).
Are Popular Diet Trends Safe While Breastfeeding?
Trendy plans can be tempting. The right move is the one that protects your energy, milk supply, and recovery.
Is a low-carb diet safe for breastfeeding mothers?
Moderate low-carb eating can be safe if it includes enough calories, vegetables, fruit, and protein. Very low-carb plans are risky because they may trigger lactational ketoacidosis, a rare condition where acids build up in the blood when carbs are too low.
Most nursing parents need at least 500 extra calories a day. If you lower carbs, replace them with produce, beans, and healthy fats, not just protein alone. If energy drops or supply dips, add back quality carbs like oats, brown rice, or sweet potatoes.
Work with a clinician or dietitian before making big changes to carbohydrates during lactation.
Can breastfeeding moms try intermittent fasting?
Intermittent fasting is not recommended while breastfeeding. There is limited safety data on milk supply and nutrient status (Hart et al., 2022).
Spreading food across the day supports steady energy and stable supply better than long gaps. Balanced meals and snacks often work better for postpartum weight loss than fasting windows.
Are other restrictive diets safe during breastfeeding?
Crash diets and plans that remove whole food groups can cut essential nutrients and reduce milk output. Fast loss also tends to come from water and muscle, which can rebound later.
If a plan promises very quick results, be cautious. Many parents report low energy and a drop in supply within weeks on severe diets. Choose steady changes, and seek guidance before any restrictive plan.
Supplements, Shakes, and Weight Loss Medications
Many products promise fast results. Safety during lactation comes first, since what you take can reach your milk.
Are weight loss supplements and medications safe while breastfeeding?
Most weight loss pills, powders, and injections are not advised during breastfeeding. Ingredients and doses are often unclear, and some can enter milk or affect supply (Campbell et al., 2024).
Prescription options may cause side effects like nausea or diarrhea, and some can lower appetite too much. Always talk with your healthcare provider before using any over-the-counter or prescription product for weight loss.
Food-first strategies are safer for both you and your baby during the first year after birth.
What natural alternatives support postpartum weight management?
Focus on a balanced plate, regular movement, and enough sleep. These core habits support steady fat loss without risking milk production.
Center meals on produce, whole grains, lean proteins, and healthy fats. Add gentle cardio and two short strength sessions each week. Keep a water bottle nearby throughout the day.
Many parents lose 10 to 15 pounds across the first year using these steps, with fewer ups and downs than quick fixes.
Balancing Weight Loss Without Affecting Milk Supply
You can lose weight after pregnancy without harming supply. The secret is slow progress, steady meals, and careful monitoring.
How to avoid drastic calorie deficits during breastfeeding?
Keep daily intake at or above 1,800 calories unless your clinician gives a different number. Severe cuts can drain energy and reduce milk output.
Plan three meals and two snacks to spread fuel across the day. If supply dips, increase calories and fluids for several days, and reduce workout intensity.
Tracking hunger, energy, and diaper counts for a short time can help you find your sweet spot.
What signs indicate your milk supply might be affected?
Watch for fewer wet diapers, fewer bowel movements, or slower infant weight gain. After the first week, most babies have about six or more wet diapers daily.
Your baby may seem less satisfied after feeds or nurse more often. If you see these signs, eat a bit more, rest, and contact your pediatrician or a lactation consultant.
Adjusting calories upward by a few hundred for several days often helps supply rebound.
Lifestyle Tips to Support Postpartum Weight Loss
Small daily choices build momentum. Think of these as gentle anchors that support your body and mood.
How do sleep and stress affect postpartum weight loss?
Short sleep and high stress can slow fat loss. They alter hunger hormones and steer choices toward quick, high-calorie foods.
- Less than six hours of sleep is linked with stronger cravings and lower motivation to exercise.
- Stress raises cortisol, a hormone that encourages fat storage.
- Sleep loss disrupts leptin and ghrelin, which makes you feel hungrier.
- High stress often leads to comfort eating and skipped meals.
- Rest whenever you can. Short naps help balance hormones and support supply.
- Stress can reduce workout consistency, which lowers daily calorie burn.
- Simple stress tools, like short walks and deep breathing, can boost energy.
- Many parents notice that better sleep leads to steadier food choices the next day.
- Research supports the link between more sleep, lower stress, and better postpartum weight control.
Protecting sleep and managing stress are two of the most effective steps you can take for steady progress.
What are easy meal planning tips for new moms?
Keep food simple and repeat what works. Convenience and nutrition can live on the same plate.
- Prep quick snacks like carrot sticks with hummus, apple with peanut butter, or whole wheat toast with a hard-boiled egg.
- Eat five to six small meals daily to keep energy steady.
- Make a protein-rich breakfast to curb cravings later.
- Lean on easy staples: oatmeal with fruit, grilled chicken salads, grain bowls, or yogurt parfaits.
- Use a standing grocery list to restock healthy basics.
- Batch-cook proteins like chicken or beans once a week for fast meals.
- Carry a water bottle and sip at each feed.
- Ask family or friends to help with meal prep during busy weeks.
Freezing a few portions of soup or chili can save you on a tough day and prevent a takeout run.
How to stay consistent and patient with weight loss?
Set realistic goals and expect plateaus. Many bodies keep some fat stores until weaning, which is normal.
Target 1 to 2 pounds per week if you are breastfeeding and fueling well. Track small wins like better sleep, fewer cravings, or a longer walk. These signs show your system is moving in the right direction.
Stress can slow loss, so keep methods gentle. A steady rhythm beats short bursts that lead to burnout.
When Should You Seek Professional Help?
Sometimes you need a guide. A licensed expert can help you protect milk supply while making progress with weight after pregnancy.
How can a dietitian or healthcare provider assist postpartum?
A registered dietitian or healthcare provider can set safe calorie targets, craft meal plans, and adjust your approach if supply shifts. They can also monitor infant growth and your lab values if needed.
If you have diabetes, thyroid issues, or food allergies, personalized guidance is especially helpful. Ask about any supplement, shake, or medication before using it while nursing.
What unique challenges might require professional guidance?
If you are eating well and moving regularly but weight will not budge, talk with your provider. Thyroid problems, anemia, and certain medications can affect metabolism.
Food intolerances can limit choices and cause nutrient gaps. Postpartum depression or anxiety can affect appetite and routine. Professional help can protect both mental health and milk supply while you work on gradual change.
Benefits of Gradual Weight Loss While Breastfeeding
Steady loss supports your energy, mood, and milk quality. It is also easier to maintain for the long term.
How does gradual weight loss support long-term health?
Slow loss preserves muscle while you burn fat. That protects your metabolism and makes maintenance easier later.
People who lose about 1 to 2 pounds per week tend to keep it off better than those who follow extreme diets. You also avoid nutrient gaps that can harm recovery and supply.
Small changes practiced daily turn into lasting habits you can rely on after weaning.
Why is optimal nutrition important for your baby?
Eating nutrient-dense foods helps your body make high-quality milk. Key nutrients like calcium, iron, and DHA move from your diet to your milk and support growth and brain health.
Poor maternal intake can lower some vitamin levels in milk. A balanced plate helps your baby gain well and maintain strong immunity.
Common Myths About Breastfeeding and Weight Loss
Many myths promise quick results. Evidence shows that slow and steady is far more common and far safer.
What are common misconceptions about rapid postpartum weight loss?
- Fast loss often means water or muscle, not fat. That tends to rebound.
- Crash diets drain energy and make newborn care harder.
- Exclusive breastfeeding helps, but it is not a magic fix for instant loss.
- Social media timelines rarely match scientific data on typical recovery.
- Small, steady changes protect nutrition and milk quality.
- Deep calorie cuts can lower supply and slow infant growth.
- Extreme low-carb trends can miss nutrients needed for healing.
Many parents find that modest daily habits, not strict rules, deliver better results and more energy.
What are realistic expectations for losing weight while breastfeeding?
Expect gradual change. Exclusive breastfeeding may help you lose a few extra pounds by 12 months, but timing and totals vary a lot.
Your body may keep some changes, like a softer belly or wider hips. Focus on strength, energy, and a stable routine. A balanced diet and regular activity support slow loss without risking milk supply.
Additional Considerations for Postpartum Weight Loss
Your emotional health affects appetite, sleep, and motivation. Caring for it supports both weight goals and your milk supply.
How does emotional and mental well-being affect weight loss?
Stress, lack of sleep, and hormone shifts can lead to cravings and skipped workouts. Some parents facing postpartum depression or anxiety find it hard to meal plan or move regularly.
Ask for help early if sadness or overwhelm lingers. A support system makes it easier to keep meals balanced and avoid restrictive dieting that can harm supply.
Better emotional health makes it easier to choose nutrient-dense meals and to stay active in small, repeatable ways.
When might weight loss not be a priority after birth?
If you are healing from a complex delivery, managing a health condition, or working through mental health challenges, focus on recovery first. Stabilize feeding and daily routines before targeting weight loss.
During the first weeks, many families prioritize bonding and milk supply. Choose nutrient-rich foods and gentle movement. Save harder goals for later, once your body feels ready.
Conclusion
Losing weight while breastfeeding works best with patience, steady meals, and regular movement. Aim for slow progress, about one pound per week, and keep intake at or above 1,800 calories a day to support milk supply and energy.
Check in with your healthcare provider before starting any diet or fitness plan. This information is for education and is not a substitute for medical advice. With consistent habits and kind expectations, you can care for your body, protect your baby’s nutrition, and reach your goals over time.
FAQs
1. How many pounds can a person safely lose each week while breastfeeding?
Most experts recommend losing about one to two pounds per week during breastfeeding. This gradual loss helps protect milk supply and supports healthy nutrition for both parent and child (Institute of Medicine, 2005).
2. What type of diet is best for weight loss while nursing?
A balanced diet rich in whole grains, lean proteins, fruits, vegetables, and healthy fats supports safe weight loss. Avoid very low-calorie diets since they may reduce milk production or affect nutrient intake.
3. Does losing too much mass too quickly affect breast milk quality?
Rapid reduction in body mass can lower the amount or quality of breast milk produced (American Academy of Pediatrics). Steady changes allow the body to adjust without harming lactation.
4. Can personal experience help guide postpartum weight management choices?
Personal stories often highlight that slow progress is normal when shedding extra pounds after childbirth. Many find that focusing on good nutrition rather than strict dieting leads to better long-term results for both health and well-being.
Summary: Safe postpartum weight loss involves steady reduction in pound mass through a nutritious diet plan tailored for lactating parents. Evidence shows that slow change preserves milk supply and benefits overall health outcomes for families seeking sustainable results.







