Expert Bariatric Doctor For Bariatric Surgeries And Obesity Treatment
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
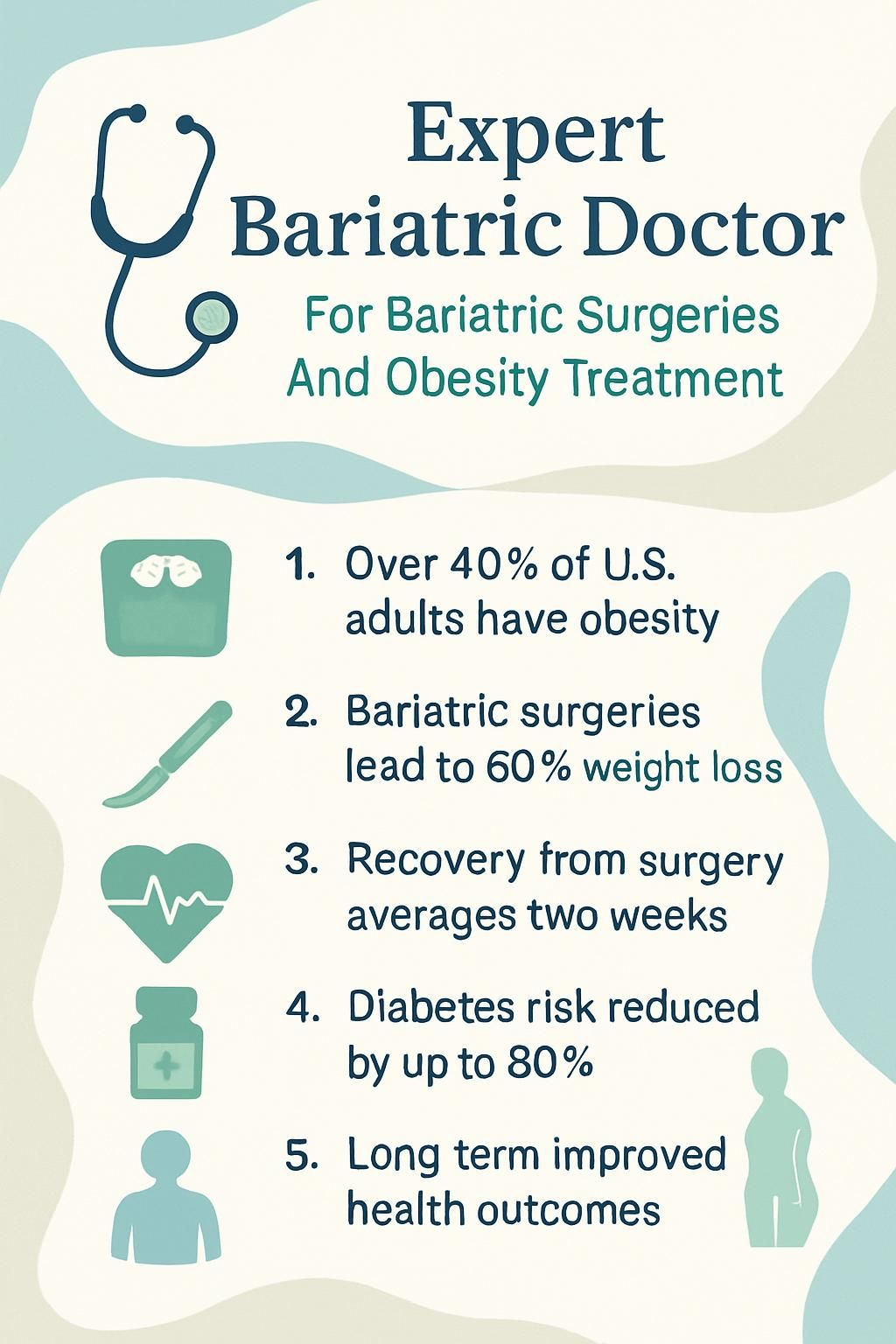
You may feel stuck if weight is hurting your health or daily life. In the United States, more than 40 percent of adults live with obesity, which raises the risk for heart disease, type 2 diabetes, and sleep apnea. An expert bariatric doctor can explain bariatric surgeries, medical weight options, and long-term weight management in plain language.
This guide offers clear answers, practical steps, and realistic expectations. Use it to plan safer choices and a steady path forward. This information is educational, not a substitute for personal medical advice.
Discover how the right care can change your future.
Key Takeaways
- Over 40 percent of U.S. adults have obesity, which raises risks for heart disease and diabetes; expert bariatric doctors treat these issues with surgery and supervised medical programs.
- Bariatric surgeries such as gastric bypass and sleeve gastrectomy can lead to about 60 percent excess weight loss in 12 to 18 months and may cut type 2 diabetes risk by up to 80 percent, based on NIH and JAMA data.
- Accredited bariatric surgeons maintain certifications from groups like the American Board of Obesity Medicine and ASMBS, which supports safer care and current skills.
- Minimally invasive procedures that use robotic or laparoscopic techniques can shorten recovery to about two weeks and lower surgical complications, according to the Cleveland Clinic.
- Regular follow-up with a bariatric specialist helps prevent nutrient gaps and supports lasting weight management after surgery or medical treatment.
What is Bariatric Medicine?

Bariatric medicine focuses on treating obesity and health problems linked to extra weight. The goal is weight loss, lower body mass index, and better health through tested methods.
What does bariatric medicine mean?
Bariatric medicine is the medical treatment of obesity and related conditions. You work with doctors who specialize in bariatrics to address extra body weight, high body mass index, and issues like diabetes or high blood pressure. Care plans include diet changes, physical activity, medication, and referrals for metabolic and bariatric surgery when appropriate.
This specialty looks at your whole health picture, not just calories in and out. Evidence-based approaches include surgery such as gastric bypass or sleeve gastrectomy if needed. Treatment aims for safe weight loss today and lower risk of serious problems tomorrow.
Why is treating obesity and related health issues important?
Obesity affects over 42 percent of adults in the United States, according to the CDC. If it is not treated, extra weight raises the risk for heart disease, type 2 diabetes, obstructive sleep apnea, some cancers, and fatty liver disease. The American Society for Metabolic and Bariatric Surgery reports that these conditions can reduce life expectancy and quality of life.
Effective treatment often improves blood pressure, blood sugar, and cholesterol levels. In my work with surgery patients who had severe obesity, I saw diabetes control improve quickly after gastric bypass or sleeve gastrectomy. Early action can help you avoid serious complications, including metabolic dysfunction–associated steatotic liver disease.
Who is a Bariatric Doctor?
A bariatric doctor specializes in obesity care and related health problems. You can expect guidance on weight loss surgery, lifestyle changes, medications, and long-term follow-up.
What does a bariatric doctor do?
A bariatric doctor evaluates your health, reviews your medical history, and checks risk factors such as body mass index, waist size, and conditions like type 2 diabetes or cholesterol problems. They perform a physical examination and may order lab tests such as glycated hemoglobin and lipid panels.
Next, the physician builds a personal plan. If you qualify for weight loss surgery such as gastric bypass or sleeve gastrectomy, the bariatric surgeon explains benefits and risks. If surgery is not your best option, the doctor may recommend weight-loss medications, nutrition counseling, and lifestyle changes. My own bariatric doctor walked me through several choices before I picked the one that fit my life.
How do bariatricians differ from bariatric surgeons?
Bariatricians provide medical treatments for obesity. They create diet plans, offer counseling for eating behaviors, and prescribe weight-loss medication. These physicians, often certified by the Obesity Medicine Association or the American Board of Obesity Medicine, do not perform surgery.
Bariatric surgeons complete training in general surgery and a bariatric surgery fellowship. They perform operations such as gastric bypass, sleeve gastrectomy, duodenal switch, and laparoscopic procedures that change the stomach or gastrointestinal tract to support major weight loss. Both specialists often work together to guide long-term care.
Next, review how several types of bariatric surgeries help treat severe overweight conditions.
Overview of Bariatric Surgeries
Bariatric surgeries help manage body weight and treat obesity by changing how your stomach and small intestine handle food. These options can lead to significant weight loss and better health.
What is gastric bypass surgery?
Gastric bypass is a weight loss surgery that changes your stomach and small intestine so you absorb fewer calories. The surgeon creates a small stomach pouch, then connects it to a lower part of the small intestine. You feel full with less food and absorb fewer calories from each meal.
Many patients lose weight quickly and see improvements in diabetes and high blood pressure. Laparoscopic Roux-en-Y gastric bypass is common, since it uses small incisions for shorter hospital stays and faster recovery compared with open surgery.
What is sleeve gastrectomy?
In sleeve gastrectomy, the surgeon removes about 75 to 80 percent of the stomach with a stapling device. What remains looks like a narrow tube, or sleeve, which limits how much you can eat. The procedure also lowers levels of ghrelin, a hormone that drives hunger.
This surgery is usually done laparoscopically, which means smaller cuts and a shorter hospital stay. Many patients with severe obesity lose up to 60 percent of their excess weight in 12 to 18 months, according to the National Institutes of Health. In my experience supporting bariatric patients, many report more energy and better health within weeks.
How does the adjustable gastric band work?
Adjustable gastric banding uses a different method. Doctors place an inflatable silicone band around the top of your stomach to create a small pouch. The pouch fills quickly, which helps you feel full sooner.
Your care team adjusts the band by adding or removing saline through a small port under your skin. These visits help control hunger and reduce calorie intake. I met a patient who found band adjustments helpful after years of stalled progress with diet and exercise alone.
What is biliopancreatic diversion with duodenal switch?
Biliopancreatic diversion with duodenal switch is a complex surgery. Surgeons create a sleeve-shaped stomach, then reroute part of the small intestine so food meets digestive juices farther downstream. This reduces calorie and nutrient absorption, which can produce major weight loss.
Patients can see large changes in body weight within two years, often with strong benefits for type 2 diabetes and severe obesity. It is not right for everyone. Doctors review medical history, past weight-loss attempts, and overall risk before recommending it.
Learning about non-surgical choices helps you understand every path to weight control and better health.
Non-Surgical Obesity Treatments by Bariatricians
Bariatricians use supervised medical care to help patients with obesity lose weight without surgery. These programs blend nutrition, activity, and prescription options when needed.
What are medical weight management programs?
Medical weight management programs combine medical oversight with nutrition, behavior coaching, and sometimes prescription treatment. A bariatric doctor tracks your progress, monitors your metabolism, and helps prevent weight regain.
- FDA-approved medications may be included when appropriate.
- Registered dietitians and mental health professionals support healthy habits.
- Regular physical activity is encouraged and tailored to your ability.
- Frequent check-ins guide shared decision-making and plan changes.
Many insurance plans now cover supervised weight loss, especially when led by a physician accredited through recognized boards or councils.
Which prescription weight-loss medications are available?
Doctors can prescribe FDA-approved medications when diet and exercise are not enough. Common options include phentermine to lower appetite and orlistat to block some fat absorption. Liraglutide and semaglutide mimic hormones that help you feel full. Bupropion-naltrexone targets brain pathways that affect hunger.
These medicines are often used if your BMI is 30 or higher, or at least 27 with obesity-related conditions. Your bariatrician will pair medication with nutrition counseling and routine check-ins. Report side effects and any changes in your health so your plan stays safe and effective.
How do nutritional counseling and lifestyle changes help?
Nutritional counseling teaches what to eat for safe weight loss and strong health. A bariatric doctor may work with a dietitian to build realistic meal plans for daily life and for life after surgery. You will learn about protein goals, hydration, and supplements to avoid nutrient gaps.
Research from the American College of Physicians shows that structured lifestyle change can help people lose 5 to 10 percent of total body weight within six months. Regular activity, such as daily walking or swimming, protects heart health and supports long-term results. Consistent follow-up helps prevent weight regain.
Choosing an Expert Bariatric Doctor
Choosing the right expert helps you get the best mix of surgery, medical treatment, and long-term support. A careful review of training and experience can save time and reduce risk.
What qualifications and certifications should I look for?
Seek a bariatric doctor who completed a residency in internal medicine, family medicine, or general surgery. Certification from the American Board of Obesity Medicine or the American Board of Surgery shows advanced knowledge in obesity care or bariatric surgery. Membership in the American Society for Metabolic and Bariatric Surgery signals ongoing education and high standards.
Your surgeon should have experience with gastric bypass, sleeve gastrectomy, and related procedures that involve the small intestine. Board certification confirms training and performance. When I searched for my specialist, I checked for accredited program involvement and recent robotic surgery training. It boosted my confidence in their skills.
How important is experience with bariatric procedures and obesity treatments?
Experience matters. A surgeon who performs many bariatric procedures understands how to tailor care, manage surprises in the operating room, and support recovery. Studies show higher-volume surgeons often report fewer complications and better outcomes.
Doctors with deep experience in obesity treatment also follow current guidelines. They can compare surgical and non-surgical options and explain likely results in clear terms. That knowledge helps you make a safer, more informed choice.
Why is personalized patient care essential?
Personalized care improves safety and results. Your doctor reviews your medical history, prior surgeries, lab results, and risks, then customizes your plan. Two patients rarely need the same strategy.
Some people require extra nutrition support after sleeve gastrectomy. Others need close heart monitoring after prior cardiac surgery. Feeling heard and involved makes it easier to follow the plan and stick with new habits.
Benefits of Working with a Bariatric Specialist
A bariatric specialist offers medical expertise, structure, and steady support. That combination can help you lose weight and protect your health for the long term.
How does a bariatric specialist support long-term weight loss?
Long-term success comes from regular follow-up, nutrition counseling, and behavior tools. Your doctor checks lab values, reviews your meals and activity, and adjusts the plan as your needs change. Some programs use monthly visits to track progress. A 2023 study found patients with monthly support lost 10 percent more weight over two years than those without it.
Specialists also connect you with support groups and helpful resources. These steps build skills to manage stress and cravings. Over time, the small wins add up.
Can bariatric specialists reduce risks of obesity-related conditions?
Bariatric specialists use proven methods, including surgery and supervised medical care, to lower disease risk. After bariatric surgery, the chance of type 2 diabetes can drop by up to 80 percent. Studies in JAMA show heart disease risk can fall by about 50 percent as weight comes down.
Many people also see improvements in sleep apnea, high blood pressure, and joint pain. During my own care, regular check-ups helped me keep blood sugar and blood pressure under control.
What support is offered to maintain a healthy lifestyle?
Support continues after surgery. Registered dietitians guide meal plans and teach portion control. Nurses review vitals and labs at follow-up visits. Support groups let you learn from others walking a similar path.
Exercise specialists build safe routines that match your current fitness level. Doctors review medications and adjust them as your weight drops. Some programs include behavioral therapy to address emotional eating and motivation. These resources make healthy habits easier to sustain.
Advanced Techniques in Bariatric Surgeries
Today’s surgical tools aim to reduce pain, shorten recovery, and improve accuracy.
What are minimally invasive and robotic-assisted procedures?
Minimally invasive procedures use small incisions and a camera called a laparoscope. Hospital stays are often shorter, and most people return to normal activities sooner than with open surgery. Robotic-assisted techniques give surgeons precise control through robotic arms controlled at a console.
These methods may reduce pain and scarring. I had robotic-assisted gastric bypass two years ago, and I was back to daily routines in about two weeks. Your surgeon will decide if these techniques fit your health and weight goals.
How do laparoscopic surgeries promote faster recovery?
Laparoscopic surgery uses small incisions and a thin camera to guide the operation. Smaller cuts can mean less tissue damage and a lower risk of infection. The Cleveland Clinic notes that most people resume daily activities within two to four weeks after laparoscopic bariatric surgery.
As a patient, I was able to walk the same day after a sleeve gastrectomy, and my scars healed quickly. Understanding your options helps you choose the approach that matches your needs.
Risks and Considerations of Bariatric Surgeries
Bariatric surgery can be life-changing, and it still carries risks. Knowing them helps you prepare and respond early.
What are the potential complications and side effects?
Common side effects include nausea, vomiting, and belly pain. Dumping syndrome can cause dizziness and diarrhea after eating sugary foods. Infection and blood clots are possible. Without proper supplements, you may develop nutrient deficiencies.
Rapid weight loss may lead to gallstones. Some people notice temporary hair thinning. Mental health shifts, including anxiety or low mood, can appear during recovery. Regular follow-up helps your team catch and treat these problems early.
Why are post-surgery follow-ups important?
Follow-up visits let your doctor track healing, weight loss, and nutrition. Studies show patients who attend scheduled visits lower their risk of deficiencies and complications by up to 50 percent. Your team can adjust medications, fluids, and supplements as your needs change.
It is also a chance to ask about activity, emotions, and long-term strategies. Skipping visits can hide warning signs of infection or internal leaks. Keep your appointments to protect your progress.
Post-Surgery Support and Care
Recovery continues at home. The right steps in food, movement, and mindset help you keep your results.
What dietary adjustments are needed after surgery?
Right after surgery, you will start with clear liquids such as broth and sugar-free gelatin. During week two, most plans move to pureed foods like mashed potatoes or blended lean meats. Solid foods return slowly after about four weeks. Choose high-protein options like eggs, fish, and lean poultry. Limit sugary and high-fat items.
Eat small portions, chew well, and take your time. Daily vitamins and minerals help prevent deficiencies, since your body absorbs fewer nutrients after surgery. My dietitian built a meal plan that matched my tastes and recovery goals, which made the process easier and safer.
What physical activities are recommended post-surgery?
Walking is usually the first activity. Begin with short, frequent walks, then increase time and pace as you feel ready. ASMBS data shows early walking reduces the risk of blood clots and speeds recovery.
Light stretching or resistance bands may come next, once your team says it is safe. Many programs suggest waiting four to six weeks before more intense exercise like swimming or cycling. Follow your care team’s advice and listen to your body.
Healthy eating and gradual activity work together to support your new weight.
How can psychological support and counseling help after surgery?
Counseling supports the emotional side of change. Mood shifts, stress, or relationship changes can surface as you adapt to new habits. Support groups and therapy offer a place to talk through setbacks and celebrate wins.
Data from ASMBS shows that people who attend counseling report higher satisfaction and steadier weight control. After my procedure, regular check-ins with a counselor helped me manage stress and stay focused on my goals.
Accredited Bariatric Programs and Clinics
Accredited programs follow strict standards. These clinics often show better safety and more consistent outcomes.
What features define reputable bariatric centers?
Strong centers feature board-certified surgeons and follow evidence-based guidelines from organizations like ASMBS. A full team supports you, including dietitians, psychologists, nurses, and patient coordinators. Education, risk assessment, and long-term follow-up are part of the process.
- Advanced surgical and monitoring technology
- Outcome tracking, including weight loss, complications, and readmissions
- Higher case volumes linked to lower complication rates
These features point to safer care and more reliable results.
Why is accreditation by medical boards important?
Accreditation shows that a center meets safety and quality benchmarks set by groups such as The Joint Commission, ASMBS, and the American College of Surgeons. Programs must follow protocols, maintain equipment, report outcomes, and keep training current.
This helps reduce complications during surgeries like gastric bypass or sleeve gastrectomy. Many insurers also prefer or require accredited centers for coverage.
Knowing what reputable centers offer helps you choose where to have surgery.
The Role of Insurance in Bariatric Treatments
Insurance often shapes your access to surgery and medical treatment. Understanding requirements can speed approval and reduce stress.
What insurance coverage is available for surgeries and treatments?
Most major plans, including Medicare and Medicaid, cover bariatric surgeries if you meet criteria. Typical requirements include a BMI of 40 or higher, or at least 35 with conditions such as type 2 diabetes or high blood pressure. Private plans may request proof of supervised weight-loss attempts.
Some policies also cover non-surgical options like medical weight programs, prescription medications, and nutrition counseling. Always check your plan, since coverage varies by state, procedure, and insurer rules.
How do I get insurance approval and pre-authorization?
Start by calling your insurer to confirm covered procedures and criteria. You will likely need medical records that show obesity-related conditions and proof of past weight-loss efforts under medical supervision. Your bariatric doctor’s office usually helps gather and submit paperwork.
Many plans require a supervised program that lasts several months. Some also request a mental health evaluation. Collect documents early, follow the checklist closely, and keep copies of everything. Steady communication with your care team and insurer improves your odds of approval.
Success Stories of Bariatric Patients
Real stories show how expert care can shift health, energy, and daily life.
What are some inspiring weight-loss journeys?
Jessica weighed 295 pounds before surgery in 2021. With guidance from an expert bariatric doctor, she chose the right procedure and joined a supervised program with nutrition and activity plans. Over two years, she lost more than 120 pounds and cut her diabetes risk by more than half.
Daniel lost 85 pounds after sleeve gastrectomy. He credits regular follow-ups, support groups, and steady lifestyle habits for maintaining both his weight loss and confidence. These stories show how accredited teams help patients reach health goals.
How does bariatric surgery impact overall health and quality of life?
Many people lose 50 percent or more of their excess weight within two years after surgery. Blood sugar improves, which can ease type 2 diabetes. Blood pressure, sleep apnea, and joint pain often improve. Research shows heart disease risk can drop by nearly 40 percent after successful bariatric treatment.
People report higher energy, better mobility, and stronger self-esteem. Medication needs may decline as weight falls and health improves. These changes support a more active life and better mental well-being.
Find out how top bariatric surgeons and clinics across the United States provide expert care in the next section.
Top Bariatric Surgeons and Clinics in the United States
Leading centers offer experienced teams, modern techniques, and long-term support to help you lose weight safely.
What services does the Denver Center for Weight Loss and Bariatric Surgery offer?
The Denver Center for Weight Loss and Bariatric Surgery provides gastric bypass, sleeve gastrectomy, adjustable gastric banding, and biliopancreatic diversion with duodenal switch. Medical weight programs include prescription options, nutritional counseling, and group support.
Pre-surgery assessments, post-operative care, and routine follow-ups help you meet your goals. Registered dietitians focus on sustainable changes, while on-site counseling supports emotional health. Insurance coordinators explain benefits and help organize approvals.
The next major provider, WellSpan Bariatric Surgery, offers its own set of care solutions for those seeking expert bariatric treatment.
What can you expect from WellSpan Bariatric Surgery?
WellSpan Bariatric Surgery features board-certified surgeons, nutritionists, and counselors. The clinic offers surgical options, including gastric bypass and gastric sleeve, and medical programs for those who are not surgical candidates.
Care begins with a detailed assessment and continues with personal nutrition and activity plans. After surgery, follow-up visits and support groups encourage long-term success. I joined a WellSpan group and found practical tips that helped me stick to my plan during recovery.
What makes UCHealth Surgical Weight Loss Center notable?
UCHealth Surgical Weight Loss Center uses modern techniques, including minimally invasive and robotic-assisted procedures. Board-certified surgeons bring years of focused experience in obesity care. The team also provides medical weight programs, nutrition counseling, and lifestyle coaching.
A friend had gastric sleeve surgery at UCHealth and received frequent check-ins and a plan that adjusted with her progress. UCHealth holds accreditation from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program, which signals strong safety and outcomes. The next section explores new directions in bariatric medicine.
Future of Bariatric Medicine
New tools and treatments aim to make obesity care safer, more precise, and easier to maintain.
What are the latest innovations in obesity treatments?
Doctors now prescribe GLP-1 medications such as semaglutide and tirzepatide, which can lead to average weight loss near 15 percent or more in adults. Endoscopic sleeve gastroplasty reduces stomach size without large incisions.
Digital health apps track eating, activity, and habits to keep you accountable. Robotic-assisted surgery improves precision and recovery time. Researchers are studying the gut microbiome to see how it shapes calorie use and weight control.
What research is ongoing in metabolic and bariatric surgeries?
Active studies aim to improve safety, cut complications, and support long-term results. Trials are testing next-generation minimally invasive procedures and faster recovery protocols. Scientists are also exploring how changes in the gut microbiome affect diabetes and weight control after surgery.
Some teams are personalizing surgery choices using genetics and health profiles. Others are pairing surgery with new medications to help keep weight off. Large registry data helps experts compare outcomes across techniques so patients can make safer, informed choices.
Conclusion
Choosing an expert bariatric doctor helps you face obesity with a clear, structured plan. The right specialist can guide you through bariatric surgeries, medical weight management, and steady follow-up care that protects your progress. Evidence from trusted groups such as the CDC, NIH, and ASMBS shows that skilled, certified teams improve safety and outcomes.
Centers like the Denver Center for Weight Loss and Bariatric Surgery, WellSpan Bariatric Surgery, and UCHealth offer comprehensive care with board certifications and experienced teams. Partner with an accredited provider to pursue lasting weight loss, better health, and a higher quality of life.
FAQs
1. What does an expert bariatric physician do for obesity treatment and bariatric surgeries?
An expert bariatric physician evaluates patients with severe weight issues, recommends suitable surgical or non-surgical treatments, and guides them through the process. These specialists use evidence-based methods to help patients achieve lasting results. According to the American Society for Metabolic and Bariatric Surgery, patients can lose 50 to 70 percent of excess body mass after surgery.
2. What types of procedures do skilled bariatric physicians offer for severe weight problems?
Skilled bariatric physicians perform several procedures such as gastric bypass, sleeve gastrectomy, and adjustable gastric banding. Each procedure has specific benefits based on a patient’s health needs. For example, gastric bypass often leads to faster initial loss of body mass compared to other methods.
3. How does an experienced bariatrics specialist support long-term success after surgery?
Experienced specialists provide ongoing care that includes nutrition counseling, physical activity guidance, and regular follow-up visits. This support helps reduce risks like nutritional deficiencies or regaining lost body mass. A study in JAMA Surgery found that structured follow-up care improves long-term outcomes in people who have had these operations.
4. Why is it important to choose a certified specialist in this field?
Choosing a certified specialist ensures that you receive care from someone with advanced training in treating severe weight conditions using both medical and surgical options. My own journey with a certified specialist led me to better understand my health risks and make informed choices about my care plan.
Summary: Expert bariatrics professionals use proven methods for treating severe weight conditions with both operations and ongoing support. Selecting a certified specialist improves safety and long-term outcomes for those seeking help with these complex health challenges.







