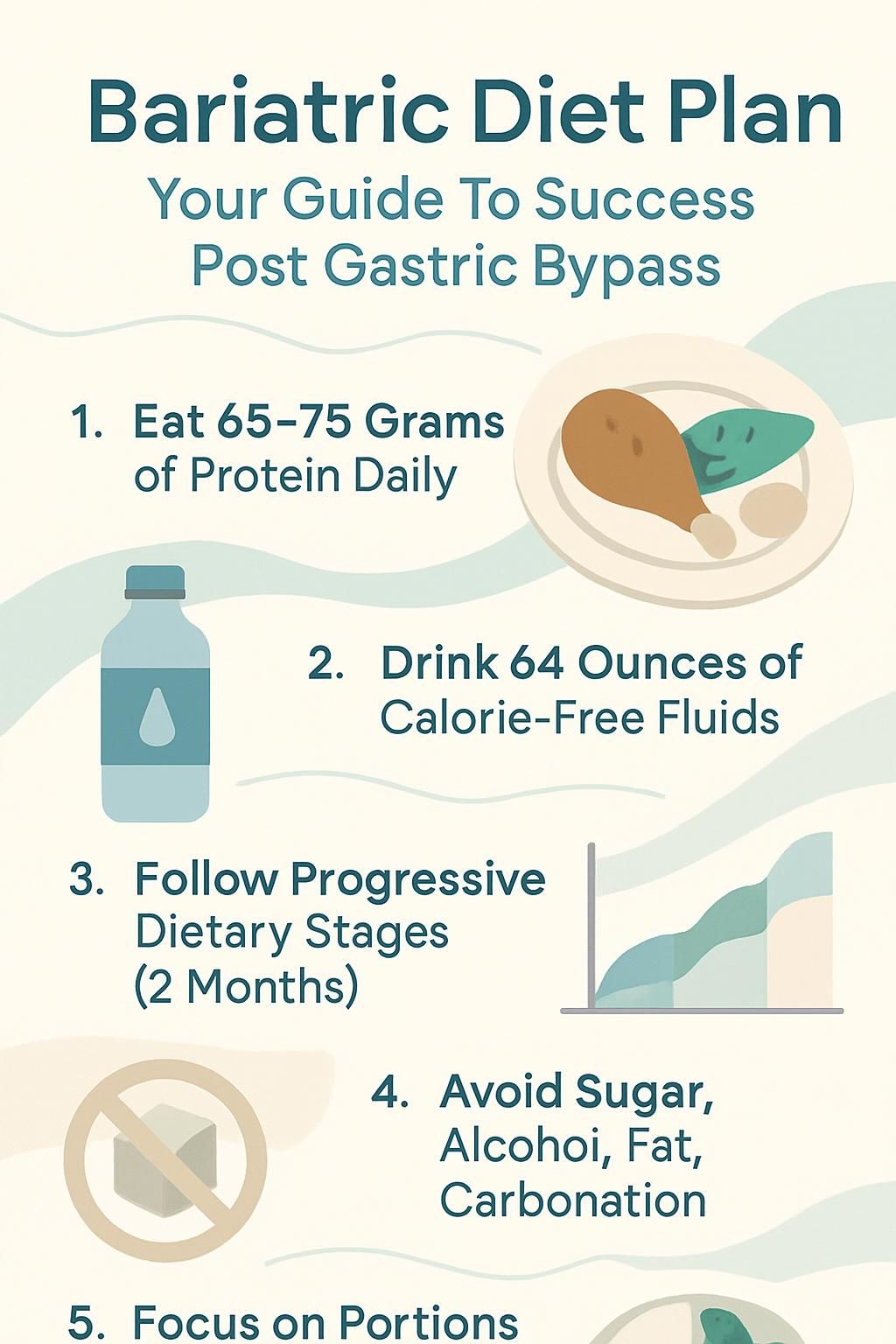
Bariatric Diet Plan: Your Guide To Success Post Gastric Bypass
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
Feeling unsure about what to eat after gastric bypass is common. Bariatric surgery changes how your stomach and intestine handle food, so a clear plan helps you heal, avoid problems, and lose weight safely.
This guide shows you what to eat, what to skip, and how to build long-term habits that fit real life. You will learn how to prevent nausea, vomiting, and dumping syndrome, and how to keep the weight off with steady, simple steps.
Key Takeaways
- Eat small, protein-rich meals, about 65 to 75 grams of protein daily, and sip 64 ounces of calorie-free fluids each day to support healing and weight loss after gastric bypass.
- Move through diet phases in order, starting with clear liquids, then full liquids and pureed foods by week 4, then soft foods and finally solids after two months, as your care team advises.
- Avoid high-sugar and high-fat foods, carbonated drinks, and alcohol to cut the risk of dumping syndrome, nausea, and weight regain, as noted by the U.S. National Library of Medicine.
- Plan on daily vitamins and minerals, including a chewable multivitamin with iron, 1,200 to 2,000 mg calcium, 800 to 1,000 IU vitamin D, and 500 mcg vitamin B12, to prevent deficiencies.
- Eat slowly, chew well, stop before you feel full, and separate fluids from meals by 30 minutes to reduce discomfort and protect your pouch.
What is a Bariatric Diet Plan?
A bariatric diet plan is a step-by-step eating guide for life after bariatric surgery. It sets portion sizes, fluid goals, and food types to protect healing, support weight loss, and prevent problems.
What is the purpose of a bariatric diet plan?
This plan limits the amount and types of food and liquid so your new stomach pouch can heal. Measured, small meals protect the pouch from stretching or damage.
Doctors and dietitians build the plan in stages. You start with clear liquids, then move to full liquids and pureed foods, then soft foods, and then solids. Each phase teaches key skills like chewing very well and choosing high-protein, low-sugar foods.
Sticking to the plan lowers your risk of nausea, dumping syndrome, and pain. It also helps prevent dehydration and weight regain. The goal is safe weight loss, good nutrition, and steady habits you can keep for life.
Over time, small, balanced meals become your new normal, which supports long-term health.
Why is it important to follow the diet plan after surgery?
Skipping your plan can lead to real problems. High-fat or high-sugar foods can cause dumping syndrome, a rapid emptying of food and liquid into your small intestine.
Eating too much or too fast may cause nausea, diarrhea, dizziness, or abdominal pain. Not drinking enough calorie-free fluids raises your risk of dehydration. Most people need at least 64 ounces, about 8 cups, daily.
Protein supports healing and protects muscle. Without the recommended vitamins and minerals, like a daily multivitamin, calcium, vitamin D, and vitamin B12, you can develop deficiencies because absorption changes after gastric bypass.
Ignoring these rules makes weight loss harder and may lead to weight regain. In some cases, poor habits can even cause a blocked pouch opening.
Following all post-surgery diet guidelines keeps you healthy while supporting safe weight loss.
Dietary Guidelines After Gastric Bypass Surgery
Clear guidelines make it easier to manage calories and digestion after surgery. Small steps protect your pouch and help you feel better as you adjust to life after surgery.
How often should I eat meals after surgery?
In the first weeks, eat 6 to 8 tiny meals a day. Space them every 2 to 3 hours. Keep portions small, about one third to one half cup, and focus on protein supplements and soft, easy-to-chew foods.
As your stomach adjusts, move to 3 to 5 small meals daily. Aim for at least one tablespoon to start, but keep any single portion under one cup. Do not drink with meals. Wait 30 minutes before or after eating to sip fluids.
This schedule helps prevent overeating and supports steady digestion.
Why is protein intake important after gastric bypass?
After surgery, your new stomach holds very little. Protein protects muscle while your body burns fat for energy.
Aim for 65 to 75 grams of protein per day in the first few months. Good options include eggs, fish, poultry, tofu, soy milk, cottage cheese, yogurt, and other low-fat dairy foods.
Without enough protein, you may lose muscle, and healing can slow. Since absorption changes after gastric bypass, make each bite count. If solids are hard to tolerate, use meal replacement shakes or soft foods like low-fat milk, yogurt, or cheese.
Which high-fat and high-sugar foods should I avoid?
Skip candy, pastries, sweetened drinks, chips, ice cream, fried foods, gravies, creamy beverages, and fruit juices. These choices add empty calories and can cause dumping syndrome.
High-calorie snacks slow weight loss. A small piece of cake once gave me sharp cramps and lightheadedness, clear dumping symptoms. Choose low-fat milk products if you want dairy, and pick lean protein over fatty processed meats.
Avoid rich sauces and desserts. These swaps help your body adapt and support long-term results.
How can I stay hydrated with calorie-free fluids?
Plan for at least 64 ounces, about 2 liters, of calorie-free fluids each day. Water is best. Decaf tea or flavored water without sugar works too.
Avoid soft drinks, juice, and alcohol. Sip between meals, not with food. Stop drinking 30 minutes before eating and wait 30 minutes after meals to resume. Carrying a water bottle helps you stay on track without feeling overfull.
Pre-Surgery Diet Preparation
Preparing before surgery makes the procedure safer and recovery smoother. A short clear liquid plan can reduce liver size and improve surgical safety.
What is the clear liquid diet phase before surgery?
This phase hydrates you and clears your gut. You will use clear liquids such as broth, unsweetened juice, decaf tea or coffee, skim or 1 percent milk, sugar-free gelatin, and sugar-free popsicles.
No solid foods or high-calorie drinks during this time. Your team may recommend this for several days or longer, based on your health. It lowers calories, supports hydration, and can reduce nausea after surgery.
How does preparing my body before surgery help?
Getting ready can shrink your liver, which helps the surgeon and lowers risks during anesthesia. Research shows a pre-surgery diet can reduce liver size by up to 20 percent.
Practice small bites, slow eating, and calorie-free fluids between meals. When I prepared, I noticed I felt satisfied with one cup of food and had fewer cravings for fatty or sugary foods.
These early habits make the post-surgery transition easier.
Post-Surgery Diet Progression
Your plan moves in careful phases. Each step protects healing, manages hunger, and teaches you how to eat with a smaller stomach.
What can I eat during the clear liquids phase (Days 1 to 3)?
Clear liquids hydrate and protect your new pouch. Keep choices simple and sugar free.
- Use broth, unsweetened juice, decaf tea or coffee, and skim or 1 percent milk in the first three days.
- Sugar-free gelatin and sugar-free popsicles add variety without extra calories.
- Take small sips every few minutes to reduce nausea and discomfort.
- Avoid caffeine to lower dehydration risk.
- Target 48 to 64 ounces, 1.4 to 2 liters, daily. Spread it out across the day.
- Skip fizzy drinks and alcohol. Carbonation irritates the pouch, and alcohol is absorbed faster.
- No solids, raw vegetables, rice, bread, or high-fiber foods. These can cause blockage or vomiting.
Next, see how often to eat as you move forward after gastric bypass.
What are examples of full liquids and protein shakes (Days 4 to 14)?
Full liquids add protein for healing. Keep portions small and watch for tolerance.
- Drink nonfat or 1 percent milk if you tolerate lactose, aiming for at least 12 ounces daily in small servings.
- Choose lactose-free or soy-based options if you have dairy issues.
- Use sugar-free pudding or yogurt in small portions to reduce dumping risk.
- Include low-fat cottage cheese or strained, blended broth-based soups for extra protein.
- Add high-protein, low-calorie liquid supplements, about 60 to 80 grams of protein per day if your team advises.
- Start with one tablespoon per serving. Increase to two tablespoons only if you tolerate it.
- Keep total daily calories modest during this period to support safe weight loss.
- Avoid liquids with alcohol or added sugars.
- Take a multivitamin supplement every day to cover iron, calcium, magnesium, vitamin D, and vitamin B12.
- Drink calorie-free fluids between meals. Wait 30 minutes before eating again to support digestion and control hunger signals.
This phase helps prevent deficiencies and gives your pouch time to adapt before pureed foods.
What foods are allowed in the pureed and blended phase (Weeks 3 to 4)?
Pureed foods should be smooth, moist, and lump free. The goal is comfort and steady protein.
- Try lean ground meats blended with broth or skim milk to a smooth texture. Keep portions small, about 4 to 6 tablespoons.
- Cottage cheese blends well and supplies quality protein.
- Blend scrambled eggs until soft and smooth.
- Choose cooked cereals like oatmeal or cream of wheat mixed with water or skim milk until smooth.
- Puree soft fruits like bananas or canned peaches with unsweetened juice to avoid sugar spikes.
- Use strained cream soups made with low-fat ingredients.
- Puree cooked vegetables like carrots or green beans and thin with broth as needed.
- Drink liquids separately. Wait at least 30 minutes before and after meals.
- Use calorie-free fluids like water or herbal tea between meals to reach at least 1 liter per day.
- Avoid added sugars, nuts, seeds, skins, rice, bread, tough meats, and sticky foods that can block the pouch opening.
Blending chicken with fat-free Greek yogurt helped me meet protein goals without discomfort. Small bites and slow eating kept nausea away.
Which soft foods are recommended (Weeks 5 to 8)?
Soft foods help you practice chewing and portion control while you heal.
- Use ground lean meats like turkey or chicken for protein. Skip tough cuts.
- Choose flaked fish like salmon or tilapia for moist texture.
- Soft or scrambled eggs offer high-quality protein.
- Low-fat cottage cheese gives protein and calcium.
- Cooked cereals such as oatmeal or cream of wheat, without added sugar.
- Small portions of rice only if tolerated well.
- Canned fruit without skins or seeds, packed in juice, not syrup.
- Soft-cooked vegetables without skins, like carrots or squash, chewed well.
- Keep each meal to one third to one half cup.
- Separate food and drinks by 20 to 30 minutes to reduce nausea.
Next, learn how to move from soft foods to solid foods safely.
How do I transition to solid foods after surgery (Months 2 and beyond)?
After about two months, you can begin solids. Introduce foods slowly and watch for signs of intolerance.
- Start with small portions, about 1 to 1.5 cups per meal, three times per day.
- Test one new food at a time. This helps you spot triggers of dumping syndrome.
- Anchor each meal with lean protein like fish, poultry, or beans.
- Use caution with bread, raw or fibrous vegetables, tough meats, fried foods, and very spicy dishes.
- Limit high-sugar and high-fat choices to prevent nausea and dumping.
- Avoid carbonated drinks and alcohol, which can cause bloating or discomfort.
- Stop eating before you feel full to protect the pouch.
- Sip calorie-free fluids between meals, and pause 30 minutes before eating.
- Chew every bite to a smooth texture and eat slowly.
- Track tolerance in a food diary to learn what works best for you.
Solid foods add variety back to your routine, but portion control stays crucial.
Key Eating Habits for Long-Term Success
Simple habits make a big difference. Think of them as guardrails that keep you steady on your new path.
Why should I eat slowly and chew thoroughly?
Slow eating lowers your risk of dumping syndrome and helps your brain catch up with your stomach. Take 20 to 30 minutes for each meal.
Chew until food is a pureed texture. This protects your pouch and improves nutrient absorption. Many centers report fewer digestive issues when people eat slowly and chew well.
How do I know when to stop eating before feeling full?
Watch for early signs of satisfaction, such as relaxed breathing or less interest in the food. Stop before you feel full.
Keep portions to 1 to 1.5 cups during the solid phase. Eat slowly, rest your fork between bites, and give each meal at least 20 minutes.
Why separate food and drinks by 20-30 minutes?
Space drinks and meals to avoid overfilling a small pouch that holds only a few tablespoons right after surgery. Waiting 20 to 30 minutes helps prevent dumping.
Drinking with meals can push food into the intestine too quickly, which may cause nausea or diarrhea^1^. Separating fluids also supports better nutrient absorption and steady hydration between meals.
Why should I avoid using straws after surgery?
Straws pull extra air into your stomach. That air can cause bloating, gas, and pressure in a sensitive pouch.
Some people notice more burping or tightness after using a straw. Small changes like skipping straws, carbonated drinks, and chewing ice can help you heal with less discomfort.
Essential Vitamins and Supplements
Your body absorbs fewer nutrients after gastric bypass. Daily vitamins and minerals help close the gap and protect your bones, blood, and nerves.
Which multivitamins are recommended after gastric bypass?
Use a high-potency chewable multivitamin each day. Look for at least 18 mg iron and 400 mcg folic acid, plus trace minerals like selenium, copper, and zinc.
Many teams suggest two tablets daily for the first three months, then one tablet daily after that. I used a chewable each morning with water, which made the routine simple and steady.
Why do I need calcium supplements?
Calcium protects your bones. Absorption drops after surgery, so most people need 1,200 to 2,000 mg per day.
Take 500 to 600 mg at a time for better absorption. Calcium citrate is often preferred because it absorbs well even with lower stomach acid. Pair calcium with vitamin D for best results.
How do Vitamin D and Vitamin B12 support recovery?
Vitamin D helps your body absorb calcium and maintain bone strength. Many providers recommend 800 to 1,000 IU daily, often split into two doses.
Vitamin B12 supports healthy nerves and red blood cells. A common routine is 500 mcg daily, by tablet or under the tongue. Consistent use supports energy and lowers the risk of anemia.
What other supplements might I need?
Some people need extra iron and folic acid, especially if they menstruate. Others may need zinc or copper if lab tests show low levels.
Work with your care team and check labs regularly. Adjustments based on results keep your plan safe and effective.
Foods to Avoid Post-Surgery
Certain foods can trigger symptoms or slow progress. Smart choices keep recovery smoother and weight loss steady.
Which high-fat and high-sugar foods should be avoided?
Avoid concentrated sweets like pastries, candy, and sugary drinks. Skip high-fat foods such as fried foods, chips, gravies, and ice cream.
These items raise dumping risk and slow weight loss. Even small portions can be a setback. Choose nutrient-dense foods that support your plan.
Why avoid fizzy drinks and alcohol?
Carbonated drinks add air to your pouch, which can cause pain, bloating, and pressure. I tried a small soda one month after surgery, and the bloating made it hard to even sip a protein shake.
Alcohol enters the bloodstream faster after surgery. A small amount can lead to stronger effects and safety risks, including impaired driving. It also adds empty calories that can hinder weight goals.
What foods cause discomfort or dumping syndrome?
High-sugar and high-fat foods are common triggers. Many people experience dumping in the first year after surgery. Symptoms include nausea, cramping, dizziness, sweating, and diarrhea.
Sticky bread, dense grains, or poorly chewed foods can also cause pain or blockage. Be cautious with items that have more than 10 grams of added sugar per serving, including sweetened shakes and condiments.
Sample Post-Surgery Meal Plan
A sample plan can remove guesswork. Use it as a starting point, then adjust with your dietitian.
What are example daily meals for Weeks 2 to 8?
- Morning, 1/4 cup hot cereal mixed with nonfat milk for a smooth texture.
- Mid-morning, 1/2 cup nonfat milk blended with a tablespoon of dry milk powder for extra protein.
- Lunch, 2 scrambled egg whites or 1/4 cup cottage cheese.
- Early afternoon, 1/2 cup low-fat chicken noodle soup or 1/4 cup sugar-free yogurt.
- Dinner, 2 ounces lean ground meat with 1/4 cup pureed or cooked vegetables.
- Before bed, 1/4 cup nonfat milk for extra calcium and hydration.
- Space 6 to 8 small feedings every two hours to stay comfortable.
- Keep total daily calories modest during this stage, as your team recommends.
What meals are suitable for long-term maintenance?
- Plan three balanced meals a day with one or two small snacks if needed. Many people aim for 900 to 1,000 calories per day.
- Get at least 60 grams of protein daily. Try grilled chicken, scrambled eggs, tofu stir-fry, or baked fish with soft-cooked vegetables.
- Keep portion sizes small, about 1/4 cup solids and 1/2 cup liquids at each meal if that is your tolerance.
- Add cooked vegetables like carrots or green beans. Avoid raw produce with skins if it causes issues.
- Use easy-to-digest grains like oatmeal or small amounts of brown rice. Limit breads, popcorn, dried fruits, and tough red meats.
- Pick low-fat dairy, such as cottage cheese or low-sugar Greek yogurt, for snacks.
- Sip calorie-free fluids through the day, but separate drinks from meals by 20 to 30 minutes.
- Avoid fried foods, sweets, sugary desserts, sodas, alcoholic drinks, and anything fizzy.
- Introduce new foods slowly based on your tolerance, and adjust protein supplements as variety improves.
- Track your intake with a diary or app to monitor protein and reinforce healthy routines.
Benefits of Following a Bariatric Diet Plan
Sticking with your plan gives your body what it needs while helping you manage your weight. It also lowers the chance of side effects.
How does the diet promote healthy weight loss?
Early on, calories are very limited, then rise to a maintenance level that supports steady loss. Small, frequent meals prevent overeating and help control hunger.
Protein keeps you full and protects muscle. Avoiding high-fat and high-sugar foods cuts extra calories that slow progress. Structured portions make cravings easier to handle.
How can it prevent nutritional deficiencies?
Daily supplements cover common gaps after surgery. A multivitamin often covers iron and zinc. Calcium plus vitamin D protects bones. Vitamin B12 supports nerves and blood cells.
Protein foods, such as eggs, fish, and Greek yogurt, also help healing and muscle strength. Together, these steps protect your health while you lose weight.
What overall health improvements can I expect?
Many people see better blood sugar, cholesterol, and blood pressure. A strong plan supports healing and makes digestion more comfortable.
Energy and mobility often improve as weight drops. Many report less sleep apnea and reduced joint pain. Following your plan supports lasting health gains.
Common Challenges and How to Overcome Them
Cravings, portions, and emotions can all get in the way. Simple tools help you stay consistent without feeling deprived.
How can I manage cravings after surgery?
- Include protein at every meal and snack to stay satisfied.
- Cut added sugars and processed snacks to reduce sweet cravings.
- Plan meals ahead to avoid impulse choices.
- Drink water or calorie-free fluids often. Thirst can mimic hunger.
- Keep quick, healthy snacks on hand, like sliced vegetables or low-fat string cheese.
- Follow the portion guidance from your care team.
- Use mindful eating. Sit down, slow down, and notice your cues.
- Track mood and triggers in a food diary. Deep breathing helped me manage stress cravings.
- Stay active with light daily movement to curb boredom eating.
- Seek support from a dietitian or a bariatric group if cravings feel strong.
These steps help you control cravings and protect long-term results.
How do I stay consistent with small portion sizes?
- Begin with 1 tablespoon portions right after surgery. Increase to 1/4 to 1/2 cup only if tolerated.
- Use small plates, bowls, and baby spoons to limit bites.
- Set a 20 to 30 minute timer and chew each bite very well.
- Log meals and snacks with exact portions for accountability.
- Measure servings with spoons and cups, not by sight.
- Pause between bites and put the utensil down.
- Limit distractions so you can focus on your hunger cues.
- Practice mindful eating to feel satisfied with less.
- Pre-portion snacks into small containers.
- Daily journaling kept my portions steady and stress lower.
These habits make smaller portions feel normal, which supports weight loss.
What strategies help control emotional eating?
- Schedule regular meals and snacks to prevent intense hunger.
- Track food and mood to spot patterns and triggers.
- Use non-food coping skills like walking, phoning a friend, or deep breathing.
- Keep tempting high-fat and high-sugar foods out of reach at home.
- Eat mindfully. Sit down, slow your pace, and chew thoroughly.
- Lean on family, friends, or a counselor trained in bariatric care.
- Celebrate progress with non-food rewards to reinforce healthy habits.
Tips for Dining Out Post-Surgery
With a little planning, you can enjoy restaurants and stay on track. Think simple preparation and small portions.
How do I choose bariatric-friendly menu options?
Pick grilled, baked, or steamed protein like chicken or fish. Ask for no added fats or sugars. Choose cooked vegetables for easier digestion.
Request a to-go box at the start and portion your meal right away. Asking how dishes are prepared also helps you avoid hidden calories.
What are effective portion control tips when eating out?
Order your entree and instantly portion out 1/4 to 1/2 cup for yourself. Place the rest in a takeout container before you start eating. Using an appetizer plate can help keep your portion separate.
Restaurant servings are often two to three times larger than you need. Eat slowly to notice fullness and stop early. Keeping your chosen portion visible makes it easier to leave the rest.
Long-Term Lifestyle Changes
Lasting change comes from daily choices. Nutrition and movement work together like a simple rhythm you can keep.
Why is regular physical activity important?
Activity helps maintain weight and protects muscle. The CDC suggests at least 150 minutes of moderate activity each week, such as brisk walking.
Movement can lift your mood and energy. Short daily walks helped me manage stress and stick with my eating plan after surgery.
How do I balance meals with protein, vegetables, and fruits?
Start with lean protein, like skinless chicken, fish, eggs, or low-fat dairy. Many programs suggest 60 to 80 grams per day.
Add soft, non-starchy vegetables, such as spinach, zucchini, carrots, or green beans. Include small amounts of peeled fruit without seeds when tolerated.
Use a simple plate method. Half vegetables, one quarter lean protein, and one quarter fruit if space allows. Eat protein first to manage hunger and support muscle repair.
How can I track progress and stay committed?
Log what you eat and drink each day. Track calories, protein, and fluids. A notebook or app works well and keeps you focused.
Schedule follow-ups with your care team to review results and adjust your plan. A bariatric support group can provide motivation and practical ideas.
Conclusion
A clear bariatric diet plan helps you recover and lose weight safely after gastric bypass. Following each stage protects healing and builds habits you can keep.
Small meals, steady fluids, and smart food choices reduce side effects and keep your nutrition strong. Vitamins and minerals fill gaps so you feel better as you heal.
Stay mindful with portions and protein, and ask your healthcare team for help when you need it. Steady effort today can improve how you feel tomorrow. This information is educational and does not replace medical advice from your surgical team or dietitian.
FAQs
1. What is a bariatric diet plan after gastric bypass surgery?
A bariatric diet plan after gastric bypass surgery guides patients through stages of eating to help the body heal and adjust. It starts with clear liquids, moves to pureed foods, then soft foods, and finally regular foods in small portions. This plan supports weight loss, reduces complications, and ensures proper nutrition.
2. Why are protein-rich foods important after gastric bypass?
Protein-rich foods are vital after gastric bypass because they help preserve muscle mass during rapid weight loss. They also support wound healing and keep you feeling full longer, which can prevent overeating. Studies show that patients who meet daily protein goals have better outcomes.
3. How can I avoid common problems like dumping syndrome with my bariatric diet plan?
To avoid dumping syndrome, eat slowly, chew food well, and do not drink fluids with meals. Choose low-sugar options and limit high-fat foods. Following these steps helps prevent nausea, cramps, or diarrhea that may occur when food moves too quickly into the small intestine.
4. What are some tips for long-term success on a bariatric diet plan?
Long-term success depends on following portion guidelines, choosing nutrient-dense foods, and taking recommended supplements such as vitamins B12 and D along with calcium and iron. Regular follow-ups with your healthcare team ensure you stay healthy and meet weight loss goals.
Summary: A structured bariatric diet plan supports healing after gastric bypass surgery by guiding food choices through each stage of recovery. Protein intake helps maintain muscle while careful meal habits prevent complications like dumping syndrome. Consistent adherence to dietary guidelines promotes long-term health and weight management according to clinical research findings (ASMBS Guidelines 2020). Personal experience shows that planning meals ahead makes it easier to stick to these changes every day.







