Ibs Diet Plan: Managing Irritable Bowel Syndrome With Low Fodmap Diet
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
If gas, cramps, or sudden bathroom trips control your day, food can help. Irritable bowel syndrome, or IBS, affects millions and makes routines hard to manage. This guide shows you how a low FODMAP diet can support an effective IBS diet plan that reduces flares and brings steady relief.
You will learn which foods to avoid, what to eat, and how to test your triggers. The steps are simple and practical. This article is educational and does not replace medical advice from your healthcare provider.
Key Takeaways
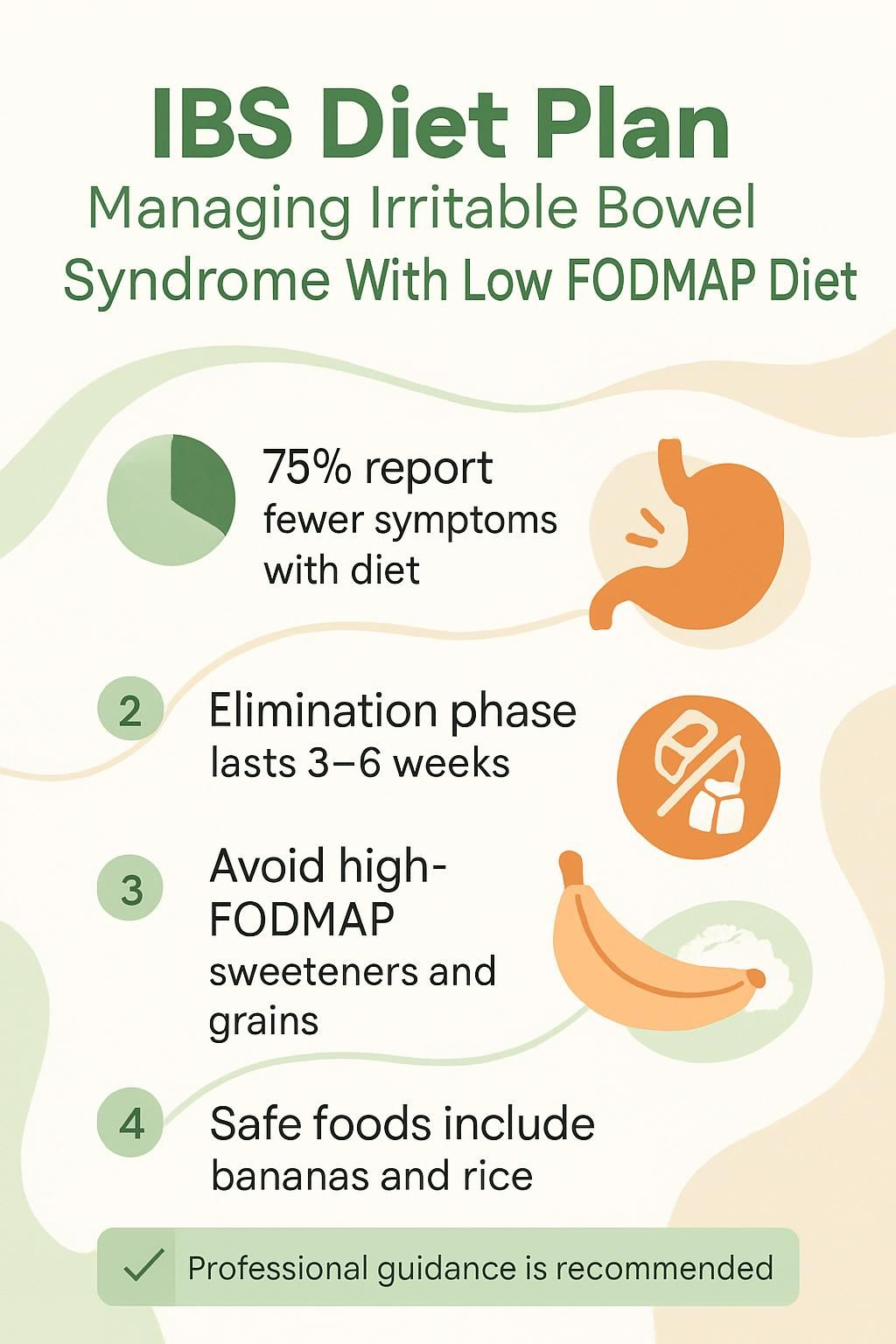
- About 75 percent of people with IBS feel better on a low FODMAP diet, including in trials such as Halmos EP et al., Gastroenterology (2014).
- The plan limits certain carbohydrates that ferment in the gut, like those in wheat, onions, apples, and some dairy, to reduce gas, bloating, and cramps.
- The elimination phase lasts 3 to 6 weeks, then foods are reintroduced to find your personal triggers for long-term control.
- Avoid high FODMAP sweeteners and some grains. Safer choices include bananas, rice, potatoes, lactose-free milk, and lean protein.
- Work with a healthcare provider or registered dietitian to keep nutrition balanced and results accurate.
Understanding Irritable Bowel Syndrome (IBS)

IBS is a common problem in the digestive system that can upset daily life. Many people feel abdominal pain, bloating, diarrhea, or constipation after certain meals. Diet changes often bring meaningful relief.
What is Irritable Bowel Syndrome?
IBS is a functional digestive disorder. That means your gut looks normal on tests, but it does not work smoothly. People notice changes in bowel habits and ongoing belly discomfort.
There is no single cure or one treatment that works for everyone. Types include IBS-D for diarrhea, IBS-C for constipation, and IBS-M if both alternate. About 10 to 15 percent of U.S. adults live with this condition according to national health estimates.
Doctors diagnose IBS based on symptoms and patterns, since no single test confirms it. Many notice symptoms after eating certain foods that act as triggers. Learning your patterns is the first step to control.
What are the Common Symptoms of IBS?
Cramping often follows meals and may last for hours. Abdominal pain can come and go, upsetting plans or sleep. Some people have diarrhea, others have constipation, and many switch between both.
Bloating and gas are very common. A sense of fullness or swelling can make normal tasks harder. Many also report frequent urges to go, changes in stool consistency, or mucus in the stool. These problems can harm quality of life unless managed with a plan, such as a low FODMAP approach.
How Does Diet Affect IBS Management?
Food choices strongly shape IBS symptoms. FODMAPs are a group of short-chain carbohydrates that are hard to absorb in the small intestine. They can trigger gas, bloating, cramps, and shifts in bowel habits.
Tracking a simple food and symptom diary helps you connect meals with flares. Common culprits include wheat, onion, garlic, beans, and milk with lactose. Cutting problem foods often brings relief. Partner these diet steps with guidance from a healthcare provider or dietitian.
Overview of the Low FODMAP Diet
The low FODMAP diet limits specific carbs that are tough to digest. Many people report fewer flares, less gas, and more predictable days after following the plan.
What is the Low FODMAP Diet and Its Purpose?
This plan was developed in Australia to help people manage IBS. FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These carbs pull water into the gut and are easily fermented by bacteria, which can trigger symptoms.
The method uses two stages. First, remove high FODMAP foods for several weeks. Next, reintroduce foods one at a time to spot your triggers. This stepwise approach helps you build a personal menu that fits your body.
Which Foods are Classified as FODMAPs?
Many everyday foods contain FODMAPs. These can set off symptoms in people with IBS.
- Wheat foods like bread, pasta, crackers, and many cereals contain fructans, a FODMAP that often causes symptoms.
- Fruits such as apples, pears, and watermelon are high in fructose or polyols and may trigger bloating or cramps.
- Vegetables like onions, garlic, cauliflower, broccoli, asparagus, and artichokes can worsen gas and discomfort.
- Legumes including beans and lentils have galacto-oligosaccharides, which ferment in the large intestine.
- Dairy such as milk, soft cheese, yogurt, and ice cream contains lactose, which can bother those with lactose intolerance.
- Sugar alcohols like sorbitol, mannitol, and xylitol, often in sugar-free gum and candy, can lead to diarrhea and discomfort.
- Processed foods with wheat flour or high fructose corn syrup raise FODMAP intake quickly, so check labels.
- Protein bars with chicory root fiber or certain prebiotics can also be high in FODMAPs for some people.
Switching from wheat cereal to rice porridge with banana or berries is one simple change many people find helpful.
Why Do FODMAPs Cause Digestive Problems?
FODMAPs are small carbs that are not well absorbed in the small intestine. They draw water into the gut, then reach the large intestine where bacteria ferment them.
This fermentation creates gas, which can cause bloating, cramping, and changes in stool. If you have IBS or small intestinal bacterial overgrowth, this process can feel intense. In a 2014 trial, 76 percent of patients reported fewer symptoms after a low FODMAP diet.[1]
Understanding how you react in each phase, elimination and reintroduction, helps you spot triggers. Small, steady changes often lead to big improvements.
…
[1] Halmos EP et al., Gastroenterology (2014): Clinical trial on Low-FODMAP Diet effectiveness
Benefits of a Low FODMAP Diet for IBS
A focused plan can calm your gut and give you back daily routines. Small shifts add up, especially when supported by good data.
How Can a Low FODMAP Diet Reduce Bloating and Cramping?
Reducing FODMAPs lowers fermentation in your gut. Less fermentation means less gas, so cramps and bloating often ease. Many also benefit from oats and up to one tablespoon of ground linseeds per day.
Avoid foods that ferment easily, such as onions, beans, cabbage, cauliflower, and broccoli. Replacing high FODMAP foods with low ones can bring relief within days. For example, removing onions from meals for one week often lowers cramps.
Can It Help Manage Diarrhea and Constipation?
Yes. The diet can support both IBS-D and IBS-C. If diarrhea dominates, limit high FODMAP fruits and sugar alcohols like sorbitol and mannitol, which can draw water into the bowel.
Constipation often improves with more fluids and soluble fiber from oats, carrots, pulses, and peeled potatoes. Increase fiber slowly to avoid extra gas. A food diary during reintroduction helps you find which FODMAP group affects you most.
How Does This Diet Improve Quality of Life?
About three out of four people report fewer symptoms after the low FODMAP plan. With less pain and more regularity, sleep often improves. Energy and confidence tend to rise when meals feel predictable.
Many people feel freer to eat out, work, or travel once they know their trigger foods. That shift can reduce stress, which helps the gut too.
High FODMAP Foods to Avoid
Some foods can push your IBS into a flare. Knowing the biggest offenders helps you shop and plan meals with less stress.
Which Fruits and Vegetables are High in FODMAPs?
These fruits and vegetables commonly trigger gas, bloating, and cramps for people with IBS.
- Fruits: apples, pears, peaches, cherries, mangoes, nectarines, plums, and blackberries often raise symptoms.
- Vegetables: cauliflower, mushrooms, asparagus, and snow peas are frequent triggers.
- Cruciferous vegetables like cabbage, broccoli stalks, Brussels sprouts, and beetroot can worsen discomfort.
- Dried fruit and fruit juice concentrates are more concentrated sources of FODMAPs.
- Artichokes and onions are rich in fructans, a key FODMAP group.
- Leeks and garlic contain fermentable carbs that disrupt digestion for many.
Many people struggle with apples and cauliflower before they start the plan. Tracking each food helps you identify your unique triggers.
What Dairy Products Contain Lactose to Avoid?
Lactose is a FODMAP found in many dairy foods. It can worsen symptoms if you are sensitive to it.
- Cow’s milk has high lactose; choose lactose-free or plant-based options.
- Cow’s milk yogurt often causes bloating; try lactose-free versions.
- Ice cream, custard, pudding, cottage cheese, ricotta, and mascarpone contain a lot of lactose.
- Ricotta and mascarpone are especially high, so swap them for lower lactose choices.
- Pudding made with regular milk can increase symptoms.
- Cottage cheese seems light, but it is not low FODMAP; pick firm cheeses like cheddar instead.
- Soft and reduced-fat cheeses often contain more lactose than hard aged cheeses.
Read labels carefully to avoid hidden lactose in mixed dishes and snacks.
What Grains Contain Gluten?
Several grains contain gluten, and many are also high in certain FODMAPs. These are usually limited during elimination.
- Wheat is a key source of fructans and can trigger symptoms.
- Rye contains gluten and fructans; avoid common rye breads and cereals.
- Barley is gluten containing and often high in FODMAPs.
- Triticale, a cross of wheat and rye, contains gluten and fermentable carbs.
- Spelt still contains gluten and can be higher in some FODMAPs.
- Farro is an old wheat variety that is not suited to this diet.
- Seitan is concentrated wheat gluten and can trigger symptoms quickly.
Choosing safer grains helps you keep fiber and vitamins in your diet without extra flares.
Why Should Artificial Sweeteners and Sugar Alcohols be Avoided?
Many artificial sweeteners and sugar alcohols are FODMAPs. They are poorly absorbed and fermented by gut bacteria, which can cause pain and diarrhea.
- Sorbitol and mannitol in sugar-free gum and candy often trigger symptoms.
- Xylitol and other artificial sweeteners can increase abdominal discomfort.
- FODMAP stands for fermentable oligo-, di-, mono-saccharides, and polyols, which includes many of these sweeteners.
- Your body absorbs only part of these sugars; the rest reach the colon and create gas.
- Processed versions often deliver higher doses than fruit, which can overwhelm your gut.
- Diets high in these additives are linked with more severe attacks.
- Even small amounts in gum or mints can cause problems for sensitive people.
- During elimination, restrict these sweeteners while you test triggers.
- For sweetness, small amounts of table sugar or maple syrup are usually tolerated better.
- Check labels. Protein bars and “lactose-free” snacks can contain polyols that upset digestion.
You may not need to avoid every sweetener forever. The goal is to limit high FODMAP options while you learn your limits.
Low FODMAP Foods to Include
There are many safe foods that make planning easier and meals more enjoyable. Think variety, color, and balance.
What Fruits and Vegetables are Low in FODMAPs?
These options work well for most people on a low FODMAP plan. Serving sizes still matter.
- Bananas, especially ripe, are safe at one medium banana per serving.
- Blueberries, cantaloupe, honeydew, kiwi, lemon, lime, oranges, grapefruit, and strawberries are usually tolerated. Keep servings around 65 grams.
- Bamboo shoots are low FODMAP and easy to add to stir-fries and salads.
- Carrots are gentle on the gut, raw or cooked.
- Cucumbers and the green tops of scallions add crunch without many FODMAPs.
- Eggplant offers fiber with low risk of irritation.
- Lettuce, such as iceberg or romaine, hydrates without triggering symptoms.
- Olives make a satisfying snack and are low in FODMAPs.
- Parsnips and potatoes provide easy-to-digest starch for energy.
Mixing these foods across meals helps reduce symptoms while keeping nutrition strong.
What are Good Lactose-Free Dairy Alternatives?
Use these choices to maintain calcium and protein without lactose issues. Check labels for added sweeteners.
- Lactose-free milk gives you the same protein and calcium without lactose.
- Almond milk is low calorie and usually low FODMAP if unsweetened.
- Rice milk is another gentle option many tolerate well.
- Hard cheeses such as feta and brie are low in lactose and easier to digest.
- Probiotic yogurt made from lactose-free milk can support gut balance.
- Soy milk made from soy protein, not whole beans, fits the plan in many brands.
- Coconut yogurt can work if unsweetened and free of high FODMAP additives.
Swapping to almond milk in coffee is a common change. Many people feel less bloated within days.
Which Gluten-Free Grains and Cereals are Safe?
Gluten-free grains can help you keep fiber without extra FODMAPs. Pair them with low FODMAP vegetables and protein.
- Oatmeal offers gentle fiber. Choose plain oats without high FODMAP add-ins.
- Rice bran supports digestion with a mild taste.
- Gluten-free pasta made from rice, corn, or quinoa digests more easily.
- Corn flour works for baking and sauces. Avoid mixes containing wheat, barley, or rye.
- Quinoa provides protein and cooks quickly.
- Buckwheat is naturally gluten-free and works as groats, cereal, or flour.
- Millet is a small seed grain rich in magnesium for porridge or sides.
Research shows these grains deliver key nutrients without driving flares.[1] Avoid wheat-based cereals during elimination to reduce cramps and bloating.
What Protein Sources are Suitable?
Protein supports muscle, energy, and repair. Choose simple cooking methods and avoid high FODMAP marinades like garlic-heavy sauces.
- Beef is FODMAP free if cooked without onion or garlic.
- Pork works well, especially lean cuts like loin or tenderloin.
- Chicken is easy to digest. Removing the skin can reduce fat-related symptoms.
- Fish such as salmon or cod adds omega-3s and supports heart health.
- Eggs are quick, affordable, and easy on digestion.
- Tofu and tempeh, when plain, are good plant proteins. Check labels for high FODMAP flavorings.
- Hard cheeses like cheddar or Swiss are low in lactose and make smart snacks.
- Nuts and seeds are portable. Limit portions of almonds, macadamia, peanuts, pine nuts, and walnuts to 10 to 15 pieces.
Building meals around these proteins makes it easier to manage IBS while staying nourished.
How to Follow the Low FODMAP Diet
A clear roadmap prevents confusion. Work step by step for the best results and fewer flares.
What is the Elimination Phase and How to Start?
The elimination phase lasts 3 to 6 weeks. The goal is to calm symptoms and set a clean baseline.
- Work with a registered dietitian or trained nutrition professional to guide you safely.
- Remove all high FODMAP foods like certain grains, lactose-containing dairy, apples, watermelon, garlic, and sorbitol.
- Keep a daily food and symptom diary. Note meals, times, and any changes like bloating, diarrhea, or cramps.
- Use allowed foods for variety, such as strawberries, spinach, carrots, rice, oats, eggs, chicken, tofu, almond milk, and lactose-free yogurt.
- Replace high FODMAP fiber sources with safe options. Consider approved fiber supplements if needed.
- Do not skip meals. Eating on a regular schedule supports steadier digestion.
- Watch weight changes. Rapid loss needs prompt attention from your provider.
- Stay in elimination for 3 to 6 weeks, then move to reintroduction with professional support.
How to Reintroduce Foods to Identify Triggers?
Reintroduction helps you learn which FODMAP groups you tolerate and in what amounts. Move slowly and test one group at a time.
- Pick one FODMAP group, like lactose or fructans, to test alone.
- Add one food from that group in a small amount for 3 days, for example half a cup of milk for lactose.
- Write down symptoms such as bloating, cramps, diarrhea, or constipation.
- Wait 2 to 3 days before the next new food to allow symptoms to settle.
- If no symptoms show on day one, increase the serving on day two and day three.
- Note differences within the same group. You may tolerate one food but not another.
- Use your results with your provider or dietitian to build a long-term plan.
- Consider fiber supplements if advised, especially for constipation.
- Keep tracking your intake and symptoms. Patterns guide smart adjustments.
What is the Long-Term Maintenance Phase?
Maintenance is your personalized plan for daily life. The aim is symptom control with a flexible, nutritious menu.
- Base your meals on tolerated foods and avoid the triggers found during reintroduction.
- Include a wide range of low FODMAP fruits, vegetables, grains, and proteins.
- Check in with your healthcare provider or dietitian to keep progress on track.
- Keep a light food diary to notice any new patterns over time.
- Adjust fiber as needed. Some people benefit from certain fiber supplements.
- Plan for travel, illness, pregnancy, or activity changes. Your needs can shift.
- Review your plan every few months. Tolerance may improve for some foods.
- Use evidence-based resources instead of untested online tips.
- Many people see fewer flares and more comfort after a steady maintenance routine.
This phase gives you freedom while keeping symptoms down with ongoing care and smart choices.
Additional Nutritional Tips for IBS
Small habits support your low FODMAP work. These tips can make daily life smoother and more predictable.
How to Increase Soluble Fiber Gradually?
Start with small servings of soluble fiber foods like oats, pulses, carrots, peeled potatoes, and ground linseeds. Add only one new source every few days to track changes.
Increase total fiber slowly, about 2 to 3 grams per week. Too much at once can worsen gas and discomfort. Try natural sources first and ask your provider about supplements if intake is still low.
What are the Best Hydration Choices?
After you increase fiber, focus on fluids. Aim for 8 to 10 cups of fluid daily, about 1.5 liters, unless your provider advises a different amount. Water should be your main drink because it supports digestion and regularity.
Choose non-caffeinated drinks like herbal tea for variety. If diarrhea is present, replace fluids promptly. Keeping a refillable bottle nearby can help you sip throughout the day. Peppermint or ginger tea may also calm the gut.
- Daily goal: 8 to 10 cups, about 1.5 liters
- Best picks: water and non-caffeinated herbal tea
- Extra focus: increase fluids during diarrhea
Why Choose Smaller, More Frequent Meals?
Meal size and timing matter. Large meals can overwork the gut and increase bloating or cramps. Smaller, more frequent meals put less strain on digestion.
Aim for three meals and two snacks each day. This pattern supports steadier energy and can reduce flares. Many people report fewer cramps after switching to this approach.
Which Foods Should be Limited for IBS?
Certain foods can make symptoms worse. Limiting them helps many people gain better control.
- Keep fresh fruit to three 80 gram servings per day to avoid excess fructose.
- High fat foods like fried items or heavy sauces can slow digestion and cause pain.
- Spicy foods may increase gut sensitivity and discomfort.
- Processed foods can contain additives that irritate the gut.
- Dairy high in lactose often causes gas and bloating for sensitive people.
- Artificial sweeteners such as sorbitol or xylitol can trigger gas and diarrhea.
- Gluten-containing grains may trigger symptoms for some people, even without celiac disease.
- Caffeine can stimulate the gut and worsen diarrhea.
- Alcohol can irritate the digestive tract and increase bloating and cramps.
Many people see fewer flares when they limit these items alongside a low FODMAP plan.
How Does Caffeine and Alcohol Affect IBS?
Caffeine speeds up bowel activity. It may lead to diarrhea or cramping. Many experts suggest capping intake at three cups of coffee or the caffeine equivalent per day.
Alcohol can irritate the lining of the gut and spark flares in sensitive people. Cutting back on alcohol and carbonated drinks can reduce gas and discomfort. Swapping evening cocktails for herbal tea is a simple change that helps many.
Special Dietary Situations
Life stages and family needs may affect your plan. A few extra steps can protect nutrition while keeping symptoms in check.
How to Follow the Diet During Pregnancy?
Pregnancy raises nutrient needs. Extra care keeps you and your baby well nourished while you manage IBS.
- Talk with your OB-GYN or a registered dietitian before starting or continuing the low FODMAP diet.
- Track iron and folate closely. Restrictive diets can make it harder to meet these needs.
- Use fortified gluten-free grains and cereals to support folate and iron intake.
- Include a wide variety of allowed fruits and vegetables for fiber and vitamins.
- Pick lactose-free dairy alternatives to meet calcium and vitamin D needs if avoiding regular dairy.
- Watch your calories. Pregnancy increases energy needs, so do not undereat.
- Stay hydrated. Adequate fluids help prevent constipation.
- Keep a food diary to spot any nutrient gaps or symptom patterns.
- Attend prenatal checkups and labs to monitor for deficiencies.
- Report rapid weight loss or persistent digestive changes to your provider promptly.
What are the Considerations for Childhood IBS?
Children have unique nutrition needs. Extra supervision helps protect growth and well-being.
- A pediatrician and a registered dietitian should oversee any low FODMAP plan for children.
- Monitor growth. Restrictive diets can affect height and weight if not planned well.
- Reserve gluten-free diets for children with a medical diagnosis, such as celiac disease.
- Keep variety across safe food groups to meet vitamin, mineral, protein, and calorie needs.
- Reintroduce foods slowly to avoid anxiety and to identify true triggers.
- Coordinate with schools and caregivers to maintain consistency.
- Offer psychological support if stress about symptoms or food avoidance is high.
- Keep portions age appropriate to prevent underfeeding.
- Seek medical advice if you see weight loss, blood in stool, or severe abdominal pain.
Teamwork among providers, families, and schools makes each step smoother and less stressful.
When to Consult a Dietitian for IBS?
If symptoms do not improve or you are cutting many foods, ask for help. Your primary care clinician can refer you to a registered dietitian.
A dietitian can guide food choices, keep nutrition balanced, and help interpret your diary. If bloating, diarrhea, or constipation persist, expert support can prevent setbacks and improve outcomes.
Common Challenges with the Low FODMAP Diet
The plan can feel strict at first. A few smart strategies make it easier to follow and easier to enjoy.
How to Identify Trigger Foods Effectively?
Use a detailed food diary. Write what you ate, the time, and any symptoms like bloating or cramps. This helps link meals to flares.
After elimination, reintroduce one high FODMAP food every three days, then watch for changes. This method improves accuracy when spotting your triggers.[1] Patterns often become clear in two to six weeks.
___
^[1]^ Monash University Low FODMAP Diet resources
How to Manage Social Situations and Dining Out?
Check menus online or call ahead about low FODMAP options. Ask for plain grilled meat, steamed vegetables without sauces, or salads with oil and vinegar. Most restaurants honor simple requests.
Carry a short safe-food list or use a trusted app. Bring a low FODMAP dish to parties so you always have one safe choice. Planning lowers stress and increases confidence.
How to Ensure Variety in Meals?
Rotate foods from different groups. Pair grains like quinoa, rice, and oats with proteins such as eggs, chicken, or tofu. Add vegetables like carrots, spinach, zucchini, and tomatoes.
Try one new recipe each week with approved ingredients. For example, make a shrimp and bok choy stir-fry one week, then gluten-free pasta with tomato and basil the next. Listing the low FODMAP foods you tolerate well can spark new ideas.
Working with Healthcare Providers
Professional support reduces guesswork and helps you stay nourished while you manage IBS symptoms. Think of your provider as your partner in the process.
When to Seek Medical Advice for IBS Symptoms?
Contact your healthcare provider if changes to your IBS diet or over-the-counter medicines do not help. Ongoing diarrhea can lead to dehydration, which needs prompt attention. Blood in stool or unplanned weight loss also needs medical review.
If pain wakes you at night or disrupts daily life despite diet steps, call sooner. A gastroenterologist can suggest tests and adjust your plan to improve control.
What Symptoms Require Urgent Attention?
Severe or sudden abdominal pain is a warning sign, especially with blood in stool or vomit. Unexplained weight loss, ongoing vomiting, high fever above 101°F, and constant diarrhea with dehydration need fast care.
If symptoms persist after a few weeks of diet changes, testing for other conditions may be needed. Early evaluation lowers risks and speeds relief.
How to Develop a Personalized IBS Management Plan?
Work with a registered dietitian who understands IBS. Use a simple log or app to track meals and symptoms. This helps you and your provider set clear goals, such as reducing bloating or improving stool frequency.
Most people see progress after 4 to 8 weeks on a supervised low FODMAP diet. Adjust the plan based on your diary and follow-up visits. A living plan works best as your needs change.
Conclusion
A structured IBS diet plan centered on a low FODMAP diet can reduce bloating, cramps, diarrhea, and constipation. Many people improve after finding their trigger foods and making targeted swaps. Studies suggest up to three quarters feel better with this approach.
Work with your healthcare provider or a registered dietitian to keep your nutrition strong while you manage IBS. With a clear process and steady tracking, you can regain comfort and enjoy daily life again without fear of sudden flares.
FAQs
1. What is a low FODMAP diet and how does it help manage irritable bowel syndrome?
A low FODMAP diet limits certain carbohydrates that can cause digestive symptoms in people with irritable bowel syndrome. Research from Monash University shows this approach reduces bloating, gas, and abdominal pain for many individuals.
2. Which foods should I avoid on an IBS diet plan using the low FODMAP method?
People following a low FODMAP plan should limit foods high in fermentable sugars such as wheat bread, onions, garlic, apples, milk products containing lactose, beans, and some sweeteners like sorbitol or mannitol.
3. Is there scientific evidence supporting the effectiveness of a low FODMAP diet for IBS?
Several clinical trials report that about 70 percent of patients experience symptom relief after adopting a structured low FODMAP eating pattern (Staudacher et al., Gastroenterology 2017). Dietitians often recommend this strategy based on these results.
4. Can you share an example of how someone might use the IBS diet plan in daily life?
After years of discomfort from frequent stomach cramps and unpredictable digestion, I tried switching to meals built around rice noodles with chicken and spinach instead of pasta dishes with garlic sauce or onion-heavy salads. Within weeks my symptoms improved; tracking food choices helped me identify which ingredients triggered flare-ups most often.
Summary:
The low FODMAP approach offers clear guidelines for managing irritable bowel syndrome by reducing specific carbohydrate intake linked to common digestive problems. Evidence supports its benefits when followed under professional guidance; personal experiences highlight practical ways to adapt everyday meals while monitoring individual responses.







