Best Diet For Diabetics: Top Meal Plan For Living With Diabetes
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
Many people struggle to find a diabetes diet that controls blood sugar and still fits daily life. You want a meal plan that keeps glucose steady and feels realistic from breakfast to dinner.
I looked to trusted sources like the Centers for Disease Control and Prevention for guidance. One point stood out in the research. Regular meals with more vegetables, whole grains, and lean proteins make managing diabetes much easier.
In this post, I share simple tips and meal planning ideas that lower stress and help you hold a steady blood sugar level. If you want a plan that works in daily life, keep reading. This is education, not medical advice. Check your choices with your healthcare provider.
Key Takeaways
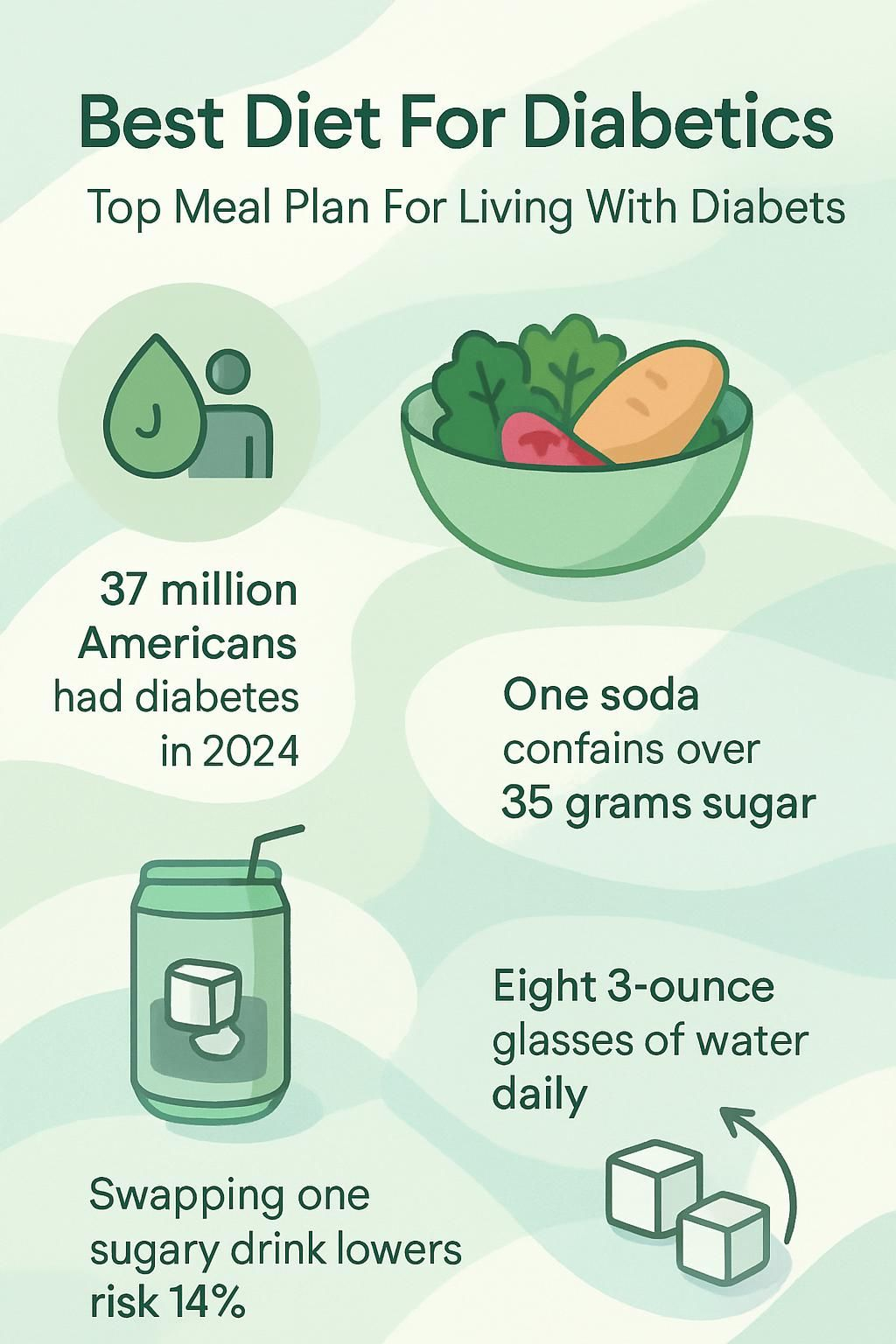
- More than 37 million Americans lived with diabetes in 2024. Regular meal timing plus whole grains, lean protein, and non-starchy vegetables supports glucose control.
- The Diabetes Plate Method from the CDC and American Diabetes Association suggests filling half your plate with non-starchy vegetables to steady blood sugar each day.
- Cutting sugary drinks lowers sharp glucose spikes. A 12-ounce soda can carry more than 35 grams of sugar.
- Plans such as the Mediterranean or DASH focus on healthy fats and plant foods. They can lower heart disease risk for people with diabetes.
- Eight 8-ounce glasses of water per day is a common goal. Swapping one sugary drink for water can reduce type 2 diabetes risk by up to 14 percent, based on Harvard research.
What is diabetes and why is diet important for managing it?

Diabetes is a chronic condition where blood glucose runs higher than normal. This happens when the body does not make enough insulin, or cannot use insulin well. Type 1 diabetes means the body makes little or no insulin. Type 2 diabetes means the body does not use insulin properly.
High blood glucose over time can harm nerves, kidneys, eyes, and the heart. Severe highs are called hyperglycemia. Lows are called hypoglycemia. The CDC estimates more than 37 million Americans have diabetes as of 2024.
Nutrition choices play a major role in daily control. A steady eating plan helps me keep energy up and hold a stable blood sugar level. Skipping planning or eating lots of added sugar often leads to spikes that strain the body.
Keeping meals at similar times improves how my insulin works, whether my body makes it or I take medicine. Experts at the National Institute of Diabetes and Digestive and Kidney Diseases support this approach.
“The foods on your plate can protect you from nerve damage, kidney disease, and heart problems linked to high blood sugar.”
Key components of a diabetic-friendly diet
A diabetes diet centers on foods that support steady glucose. I build meals with fiber-rich foods, lean protein, and heart-healthy fats for balance and taste.
Why focus on non-starchy vegetables?
Non-starchy vegetables like broccoli, carrots, peppers, and cauliflower are rich in nutrients yet low in carbs and calories. They help control blood sugar because they do not cause quick spikes.
The Diabetes Plate Method suggests filling half of a 9-inch plate with non-starchy vegetables. The fiber helps steady blood glucose and keeps me full longer.
Leafy greens like spinach and kale are “diabetes superstars,” according to the American Diabetes Association. Starting meals with a large serving of steamed green beans or a colorful salad makes my diabetes meal planning simpler.
Making vegetables the base of most meals supports weight goals and heart health. It can also help keep cholesterol in a healthy range.
How do whole grains and fiber help diabetes?
Non-starchy vegetables keep meals light and filling. I add whole grains like brown rice, oats, or quinoa to boost fiber and help manage diabetes better.
Fiber slows how fast glucose enters the blood after you eat. Oatmeal or whole wheat bread in the morning often beats sugary cereal at holding a stable blood sugar level.
Mayo Clinic reports that higher fiber intake supports lower cholesterol and a healthy weight over time. Many whole grains score low to medium on the glycemic index, which means steadier energy and fewer spikes.
Plant-based foods like beans and lentils add even more fiber. That supports digestion and helps me feel full on fewer calories.
Choosing high-fiber grains supports my digestion and helps me stay within my blood sugar target.
What are the best lean protein choices for diabetics?
Fish is one of my top lean proteins, especially salmon, mackerel, tuna, and sardines. The American Heart Association suggests two servings per week. These fish provide omega-3 fats that support heart health.
Skinless chicken breast and turkey fit well because they contain less saturated fat than many red meats. Beans, lentils, and hummus give plant-based protein with extra fiber, though I watch portions because beans contain carbs.
Eggs offer quality protein without spiking blood sugar. One large egg has about 6 grams of protein and less than 1 gram of carbs. The Plate Method places lean protein in one quarter of my plate. I bake or grill instead of frying to avoid extra unhealthy fats.
Which healthy fats should be included in a diabetic diet?
Healthy fats support cholesterol and heart health, both vital for people with diabetes. I choose monounsaturated and polyunsaturated fats from olive oil, canola oil, avocados, nuts, and seeds.
The American Diabetes Association recommends oils like olive or canola instead of butter to reduce the risk of type 2 diabetes and heart issues.
Small servings add flavor without raising glucose or pushing calories too high. One tablespoon of olive oil has about 120 calories and offers heart-friendly benefits. Avocado on whole-grain toast is one of my favorite snacks.
Why choose low-fat dairy products?
Low-fat dairy such as milk, yogurt, and cheese gives me protein and calcium without as much saturated fat. That helps me care for my bones and my heart at the same time.
I manage my weight more easily when I include low-fat yogurt or milk as part of the Plate Method. Choosing lower fat options cuts saturated fat, which supports healthy cholesterol levels.
These choices help satisfy cravings without spiking blood sugar. They also fit well with eating plans like the Mediterranean Diet or the DASH Diet.
Foods to avoid for better blood sugar control
Smart choices help keep blood glucose in a healthy range. Some foods cause fast rises and make diabetes management harder.
What sugary drinks and snacks should diabetics avoid?
Sugary drinks and snacks hit the bloodstream fast and add little nutrition. The best diets for diabetes focus on steady blood sugar through the day.
- Regular soft drinks are loaded with added sugar. A 12-ounce soda can top 35 grams of sugar, which is risky for people with diabetes.
- Fruit juices, even 100 percent juice, deliver large amounts of natural sugar without fiber. They can spike blood sugar almost as fast as soda.
- Candy, cookies, pastries, and cake use refined flour and added sugars. These make it harder to manage glucose between meals.
- Sweet breakfast cereals provide quick energy, but the added sugars and low fiber cause rapid spikes.
- Energy drinks and sweetened coffee drinks pack caffeine and high sugar. Some large coffees reach 50 grams of sugar per serving.
- Flavored yogurts and puddings with added sugar can be as problematic as candy or ice cream.
- Sports drinks often carry at least 20 grams of sugar per bottle, which can derail a careful diabetes plan.
- Sugary teas and lemonade offer empty calories. Water or unsweetened tea helps avoid needless glucose spikes.
- Dried fruits with added sugar raise carbs much faster than fresh fruit.
- Ice cream, milkshakes, and frozen desserts mix sugar with dairy fat, which is not ideal for diabetes care.
Choosing water or zero-calorie drinks supports digestion, metabolism, and long-term diabetes prevention. Less added sugar also lowers the risk of complications.
Why eliminate refined grains from your diet?
Refined grains raise blood sugar quickly and strip away valuable nutrients. A diet in diabetes should focus on foods that help keep glucose steady.
- White rice and white bread absorb fast, which can spike blood sugar within minutes.
- Processed foods often use refined grains that lack fiber, vitamins, and minerals needed for gut and kidney health.
- People who pick whole grains over refined ones may have a 20 to 30 percent lower risk of type 2 diabetes.
- Quality carbs from whole wheat or oats support steadier blood sugar than low-fiber foods.
- Swapping refined grains for whole grains supports weight loss, which helps prevent diabetes problems.
- Many refined grain foods also contain trans fats or added sugars. This raises long-term risk for several diseases.
- Replacing refined grains with whole grains fits well with guidance from a diabetes educator and supports stable glucose through the day.
How do trans fats and processed foods affect diabetes?
Trans fats and heavily processed foods make diabetes control harder. They can raise harmful cholesterol and lower the helpful kind, which raises heart risk.
- Trans fats raise LDL and lower HDL cholesterol, which can increase heart disease risk for people with diabetes.
- They are common in packaged snacks, baked goods, fried foods, and some margarines.
- Processed foods often contain added sugars that cause fast spikes in blood sugar.
- Unhealthy vegetable oils and refined grains can make glucose control more difficult.
- Many prepackaged diet meals hide sugars or trans fats, which makes them poor choices for a diabetic diet.
- Avoiding trans fats can help lower triglycerides, which supports heart health.
- My low blood sugar episodes dropped after I cut most processed snacks.
- Experts advise limiting processed foods to keep blood sugar in a healthier range.
- Choosing vegetables, seeds, lean proteins, and whole grains supports better digestive and kidney health than highly processed options.
Popular diet plans that support diabetic health
Several eating patterns can help you maintain a healthy weight and improve glucose control. I tested options and kept what worked for me.
What is the Mediterranean Diet and how does it help diabetes?
The Mediterranean diet highlights fruits, non-starchy vegetables, fish, poultry, nuts, olive oil, legumes, and whole grains. It limits red meat, butter, and salt. The focus is on healthy fats from olive oil and nuts, plus lots of plant foods.
People with type 1 diabetes and type 2 diabetes can benefit. Studies in major journals since 2015 show better blood sugar control compared with a standard Western diet.
Guidelines allow moderate wine intake, one drink daily for women and two for men. These balanced meals lower heart disease risk and may help prevent type 2 diabetes.
I use these principles to keep my portions consistent while still enjoying variety. It became a practical meal plan that works for me.
How does the DASH Diet benefit diabetics?
The DASH Diet supports people with diabetes, especially if blood pressure runs high. It includes fruits, vegetables, low-fat dairy, whole grains, lean meats like poultry or fish, beans, and nuts.
It allows small amounts of sweets, which helps me enjoy balanced meals without spikes. A 2011 study found that pairing DASH with exercise improved insulin sensitivity during weight loss.
Fiber from beans and nuts supports digestion. Limiting sugary foods protects kidney health. Managing portions using DASH principles helps me keep fasting sugars steadier without cutting out key nutrients.
Is a low-carb diet effective for managing diabetes?
Lower carb intake can help reduce high blood sugar, especially in type 2 diabetes. A review by many experts found that limiting carbs can improve glucose control.
Carbohydrate counting is personal. Not everyone needs to cut carbs sharply. Some try plans like Atkins or South Beach with medical guidance.
I tracked my carbs after diagnosis and saw improvements. The glycemic index helped me choose carbs with less impact, even when I enjoyed an occasional glass of wine with a meal.
Responses vary, but making smart carb choices supports stable blood sugar without losing key nutrients.
What are the advantages of a plant-based diet for diabetes?
A plant-based diet limits animal products and centers on whole foods. My meals carry more fiber, fewer calories, and less saturated fat than many standard diets. Fiber slows blood sugar rises and keeps me full longer.
The American Diabetes Association notes that plant-forward eating can support heart health for people with diabetes. I felt better energy when I chose non-starchy vegetables and whole grains over processed meats.
Vegetarian or vegan patterns can work well if planned carefully. I met with a registered dietitian to cover all nutrients and match my plan with my activity and therapy.
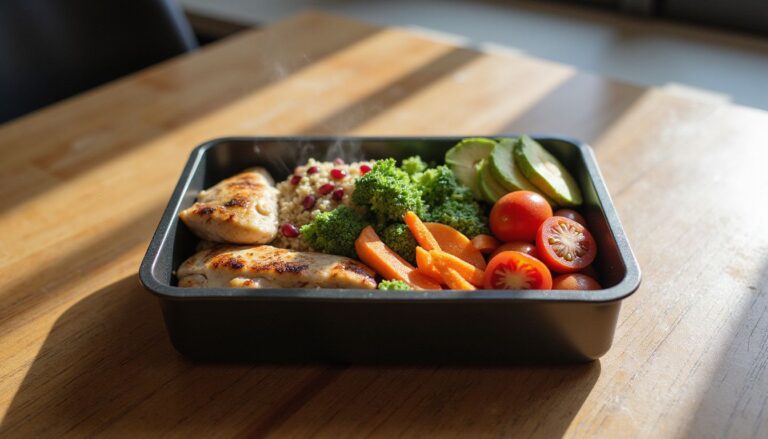
Using the Diabetes Plate Method to plan meals
I use the Diabetes Plate Method to keep my blood sugar in a healthy range. It is a simple visual guide that makes portions easy at every meal.
How to fill half your plate with non-starchy vegetables?
Non-starchy vegetables fill half of my plate. They are low in calories and carbs, which supports stable blood sugar.
- I choose spinach, carrots, peppers, tomatoes, and cucumbers for color and nutrients.
- Filling half the plate with these options lets me eat a larger volume without a spike.
- One serving is about one cup raw or one-half cup cooked for most vegetables.
- Fiber from these vegetables improves fullness and supports digestion.
- They offer vitamin C, vitamin A, vitamin K, and potassium for overall health.
- I wash and chop vegetables in advance to make adding them quick and easy.
- Roasting or steaming boosts flavor with only a teaspoon of oil.
- Salads, veggie stir-fries, and soups make it easy to hit the half-plate goal.
Whole grains and fiber also matter for blood sugar management and energy.
What should a quarter plate of lean protein include?
A quarter of my plate holds lean protein to support muscle and fullness. The right choices help keep glucose within my target range.
- Skinless chicken or turkey provides lean protein with less saturated fat.
- Tuna, salmon, or mackerel twice a week offers omega-3 fats and heart benefits.
- Beans or lentils add plant protein and fiber for steadier blood sugar.
- Tofu and tempeh serve as flexible vegetarian options.
- Eggs fit well. One large egg has about 6 grams of protein.
- Low-fat cottage cheese or Greek yogurt add protein and calcium.
How to portion a quarter plate of whole grains or starchy vegetables?
Carb portioning is key for a meal plan that supports steady glucose. Whole grains or starchy vegetables should cover one quarter of the plate.
- Use a 9-inch plate and picture four equal sections.
- Fill one section with brown rice, quinoa, bulgur, farro, or another whole grain.
- Starchy vegetables like corn, peas, or a small baked potato also fit here.
- One serving can be one-third cup cooked brown rice, one-half cup mashed sweet potato, or one slice whole-wheat bread.
- Start small if unsure. Add more based on readings and how you feel.
- Whole grains carry more fiber than refined grains, which slows glucose absorption.
- Rotate grains and starchy vegetables to keep meals interesting and balanced.
- I keep pre-portioned containers of cooked grains in the fridge for quick meals.
- Check labels on packaged grains to avoid hidden sugars and additives.
Top superfoods to support diabetes care
Certain foods make diabetes care easier. Adding them to meals can improve your numbers and your energy.
What are the benefits of leafy greens like spinach and kale?
Leafy greens carry few calories and carbs, yet deliver fiber and many vitamins. One cup of raw spinach has about 7 calories and less than 1 gram of carbs.
Spinach and kale provide vitamin K, vitamin A, vitamin C, folate, calcium, iron, and magnesium. Lutein and zeaxanthin support eye health. A 2010 BMJ study linked daily leafy greens with up to a 14 percent lower risk of type 2 diabetes.
Adding these greens helps me manage blood sugar and feel well overall.
How do garlic and onions aid diabetes management?
Garlic and onions are rich in antioxidants that may lower oxidative stress. Some 2023 studies suggest garlic can support insulin action and improve glucose control.
Onions carry quercetin, a compound linked to better fasting glucose in research. They add strong flavor without raising sodium or calories much.
Both are nutrient dense and relatively low in carbs. One hundred grams of raw onion has about 9 grams of carbs. I use them in soups, stir-fries, and roasted dishes to boost taste and nutrition.
Why include berries and citrus fruits in your diet?
Berries and citrus fruits are high in fiber, vitamin C, and antioxidants. Their natural sugars taste sweet, but a small serving usually does not cause a big spike for me.
One cup of strawberries has about 12 grams of carbs and 3 grams of fiber. A bowl of blueberries or a small orange often satisfies a sweet craving better than a cookie.
What role do nuts and seeds play for diabetics?
Nuts and seeds supply healthy fats, plant protein, and fiber. Almonds, walnuts, chia, and flax provide fats that can lower cholesterol.
A small handful keeps me full between meals without a spike. The fiber slows how fast sugars enter the blood.
Portion control matters since nuts and seeds are calorie dense. I choose unsalted options to limit sodium.
How does fatty fish like salmon and mackerel help diabetes?
Fatty fish such as salmon, mackerel, tuna, and sardines deliver omega-3 fats. Omega-3s can reduce inflammation and improve cholesterol, which is vital because diabetes raises heart risk.
I aim for two servings per week. These fish support better glucose control and heart protection while adding quality protein to a diabetic-friendly diet.
How to manage meal timing and portion sizes
Set meal times and portion sizes act like guardrails. They keep your day steady and your blood sugar predictable.
Why are regular meals important for diabetes?
Regular meals make diabetes easier to manage. Timed eating supports stable blood sugar and medication timing.
- Set meal times help prevent big spikes and drops, which lowers the risk of lows or highs.
- A steady schedule works with insulin and oral medicines, which improves control.
- Meals every 3 to 5 hours support steady energy and focus.
- Skipping meals often causes wider glucose swings.
- The Plate Method pairs well with regular intervals and consistent portions.
- Many clinicians suggest no more than 4 to 5 hours between meals.
- I had fewer severe lows after I planned breakfast, lunch, and dinner at set times.
- Routine eating helps me predict carb intake and match doses more accurately.
How to balance portion sizes effectively?
Balanced portions help with blood sugar and weight. The Plate Method plus simple tools make it practical.
- Use the Plate Method. Half vegetables, one quarter lean protein, one quarter whole grains or starchy vegetables.
- Measure foods like rice, pasta, dairy, and fruit with a scale or cups.
- Read labels for serving size to avoid hidden carbs and calories.
- Track intake in a journal to spot patterns that affect glucose.
- Plan sample menus in the 1,200 to 1,600 calorie range if helpful.
- Practice mindful eating. Slow down and notice fullness cues.
- At restaurants, split a dish or box half before you start eating.
- Work with a dietitian to adjust portions based on your readings.
Strategies to manage diabetes through diet
Small habits done often create momentum. A few simple tools can sharpen your diabetes management.
How does keeping a food journal help diabetes management?
My food journal tracks what I eat, when I eat, and how much. I also note glucose readings and activity.
Writing it down helps me connect foods with blood sugar changes. If a meal spikes me, I adjust it next time. A 2021 Diabetes Care study found that regular self-monitoring tools, including journals, supported better glucose control.
Sharing the journal with my care team improves their advice on timing and swaps. Seeing patterns on paper makes it easier to skip high-sugar snacks the next time I am tempted.
Why monitor carbohydrate intake closely?
Carbs affect blood sugar more than protein or fat. That is why carbohydrate counting sits at the center of diabetes management.
Each carb “choice” equals about 12 to 15 grams. I check labels and measure portions so my insulin and carbs match.
The glycemic index helps me pick carbs that hit slower. High GI foods spike faster, while lower GI carbs are steadier. Careful monitoring keeps my glucose within target more often.
How much water should diabetics drink daily?
Many adults aim for about eight 8-ounce glasses of water per day, close to 64 ounces. Water helps prevent dehydration and supports healthier blood sugar levels.
My numbers run steadier when I pick water or zero-calorie drinks instead of sugary options. Harvard data shows replacing one sugary drink daily can cut type 2 diabetes risk by up to 14 percent.
If you are active, live in a hot climate, or take diuretics, you may need more. Dehydration can raise glucose and add strain on the kidneys.
Why should meal skipping be avoided?
Hydration supports stable readings, but regular meals matter just as much. Skipping breakfast or lunch can drop my glucose too low, then I overeat and spike later.
Skipping also changed how well my meds worked. Research suggests irregular eating patterns can raise complication risk. Keeping meals consistent protects control and keeps me feeling steady through the day.
How can exercise support a diabetic diet?
Exercise works like a partner to your meal plan. It helps your body use insulin better and keeps energy up.
What are the benefits of physical activity for diabetics?
Regular movement improves how the body uses insulin, which supports better blood sugar control. Studies show activity can lower A1C and sometimes reduce medication needs.
Exercise also supports heart health, an area of higher risk with diabetes. Daily walking keeps my readings steadier throughout the week.
The American Diabetes Association suggests at least 150 minutes per week of moderate activity. That can make a real difference.
Which exercises are recommended for people with diabetes?
Aerobic activity and resistance training are the top picks. Choose activities you enjoy so you will stick with them.
- Brisk walking for 30 minutes, five days a week, supports heart health and insulin sensitivity.
- Swimming is low impact and joint friendly. I swim laps or take water aerobics.
- Cycling outdoors or on a stationary bike offers cardio without pounding the joints.
- Resistance training with light weights or bands twice a week builds muscle and improves glucose control.
- Yoga improves flexibility, balance, and stress, all helpful in diabetes care.
- Dancing boosts fitness and keeps motivation high.
- Gardening provides gentle movement while reducing stress.
- Check blood sugar before and after exercise to avoid lows.
- Consult your clinician to make sure your plan fits your health status.
Creating a personalized meal plan for diabetes
A personalized meal plan makes daily decisions easier. I feel calmer about food when my plan matches my life and goals.
When should you consult a registered dietitian?
I book a registered dietitian visit when my blood sugar becomes hard to control or labels confuse me. A dietitian can tailor a plan to my medication schedule and lifestyle.
During one visit, I learned how to measure servings and read labels for total carbs, fiber, and added sugar. Dietitians follow current guidance from the American Diabetes Association.
It is especially helpful when starting new medicines, managing weight changes, planning a pregnancy, or after a new diagnosis. Many insurance plans cover these services because they improve outcomes and reduce stress.
How to tailor your meal plan to your lifestyle and goals?
After working with a dietitian, I adjusted my plan to fit my culture, schedule, and tastes. The goal is to make healthy choices feel natural.
- List goals like weight loss, heart health, or stable blood sugar to guide food choices.
- Choose familiar foods from your culture to improve satisfaction and consistency.
- Match meal timing to work, school, and family so you do not miss meals.
- Make gradual changes. Small steps are easier to maintain long term.
- Use the Plate Method to manage portions and track easily at each meal.
- Include favorite healthy foods to prevent cravings for less healthy items.
- Watch how meals affect your readings and tweak recipes or snacks.
- Batch cook on weekends if weekdays run busy. Keep healthy options ready.
- Plan regular water breaks. Hydration supports appetite control and metabolism.
- Revisit the plan every few weeks. Adjust as your needs or goals shift.
These steps helped me control diabetes without giving up the foods and traditions I value.
What are common myths about diabetic diets?
Myths add confusion and make planning harder. Clearing them up opens the door to a more flexible and enjoyable plan.
What misconceptions exist about sugar and carbohydrates?
Some say people with diabetes must cut all carbs. The truth is that quality and portion size matter most. Whole grains, legumes, fruits, and vegetables provide fiber that helps manage blood glucose.
I once feared eating carbs, but my dietitian taught me how to portion them well. Sweet fruits can fit if I watch serving size.
Another myth says honey is safer than table sugar. Both raise blood sugar in similar ways, according to the American Diabetes Association.
How to understand “diabetes-friendly” food labels?
Front labels can mislead. Products that claim “diabetes-friendly” may still contain added sugars or long ingredient lists.
I focus on the Nutrition Facts panel and ingredients. Some meals marketed to people with diabetes hide sugars under names like maltodextrin. Checking with a clinician or dietitian helps me make better choices.
Additional lifestyle changes to improve diabetes management
Healthy routines outside the kitchen matter. Small daily habits can improve control and quality of life.
How does managing stress affect diabetes?
Stress can raise hormones like cortisol and adrenaline, which may push blood sugar higher. It can also raise blood pressure.
Simple practices help. I use deep breathing, short walks, or stretching to steady my mood. Research shows better stress control can reduce complications and improve daily glucose.
Why is quality sleep important for diabetics?
Good sleep supports healthy blood sugar levels. Too little sleep can raise fasting glucose and reduce insulin sensitivity.
One study found adults sleeping under six hours had higher fasting glucose than those who got enough rest. A consistent schedule helps me keep energy stable and manage symptoms more easily.
Conclusion
Choosing the best diets for diabetes helps you manage blood sugar, protect your heart, and support a healthy weight. Build meals around whole grains, lean proteins, non-starchy vegetables, and healthy fats for steady energy.
Limit sugary drinks and processed foods to prevent sharp spikes. Regular meal times and portion control make your plan easier to follow. A registered dietitian can help you shape a practical meal plan that works for your life.
This is general information, not individual medical advice. Work with your healthcare team to personalize your diabetes diet for your goals and health needs.
FAQs
1. What is the best diet plan for people with diabetes?
A balanced meal plan for individuals living with diabetes includes whole grains, lean proteins such as poultry or fish, non-starchy vegetables like broccoli and spinach, healthy fats from sources like olive oil or nuts, and limited added sugars. Research shows that eating high-fiber foods helps control blood sugar levels and supports heart health (American Diabetes Association).
2. How many carbohydrates should a person with diabetes eat each day?
Most experts recommend 45 to 60 grams of carbohydrates per meal for adults managing diabetes; however, needs can vary based on age, activity level, and medication use. Tracking carbohydrate intake helps maintain stable glucose levels throughout the day.
3. Are there specific foods diabetics should avoid in their daily meals?
People living with diabetes should limit processed snacks high in refined sugars such as pastries or soda drinks; they also need to reduce saturated fat found in fried foods and fatty meats. Consuming fewer sugary beverages lowers risk of blood sugar spikes according to recent clinical studies.
4. Can you share an example of a daily diabetic-friendly menu?
Yes; breakfast could be oatmeal topped with berries and walnuts while lunch might include grilled chicken salad with mixed greens plus vinaigrette dressing. For dinner try baked salmon served alongside quinoa and steamed green beans. This approach keeps energy steady across meals which I have found helpful when supporting family members who manage type 2 diabetes.
Summary: A well-structured diet plan focusing on fiber-rich grains, lean protein choices like fish or poultry, plenty of vegetables such as spinach or broccoli along with healthy fats aids those living with diabetes by promoting stable blood sugar levels while reducing risks linked to poor nutrition habits.