Ultimate Heart Healthy Diet Plan: Boost Your Heart Health With This Eating Plan
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
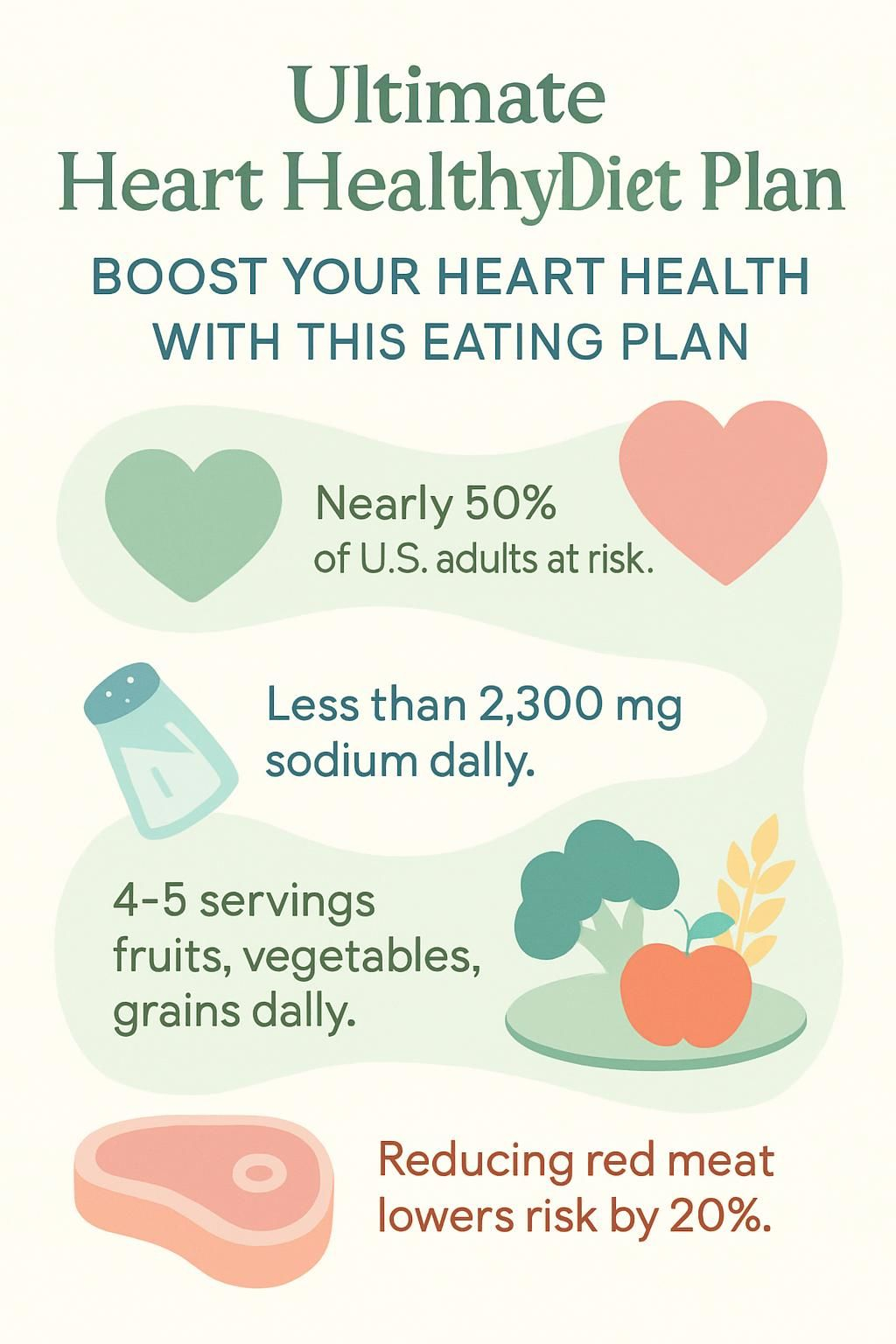
If you worry about your heart health or have a family history of heart disease, you are not alone. A heart-healthy diet gives you control over daily choices that affect long-term risk. Nearly half of adults in the United States have at least one major risk factor for heart problems.
Through careful research, I shaped an evidence-based eating plan that helps lower cholesterol, reduces high blood pressure, and supports lifelong cardiovascular health. The trusted DASH Eating Plan and American Heart Association guidance shaped many of these steps.
In this blog, you will find step-by-step meal ideas, practical grocery tips, simple label-reading skills, and science-backed advice you can use today. Small changes add up, and we can start right now.
Key Takeaways
- Almost half of U.S. adults have at least one risk factor for heart disease, so a heart-healthy diet is key for prevention and everyday control.
- The DASH Diet, ranked the #1 Heart-Healthy Diet by U.S. News & World Report in 2025, targets under 2,300 mg sodium per day and limits saturated fat to under 6 percent of calories.
- Four to five daily servings of fruits and vegetables plus whole grains can lower cholesterol and steady blood pressure, according to the American Heart Association and NIH.
- Replacing red or processed meat with poultry or plant protein can cut heart disease risk by up to 20 percent in clinical studies.
- Regularly eating fatty fish rich in omega-3s, nuts, seeds, legumes, olive oil, and low-fat dairy supports cardiovascular health, echoing Mayo Clinic and DASH guidance.
What is a heart-healthy diet?

A heart-healthy diet centers on foods that lower the risk of cardiovascular disease and protect the heart and blood vessels. In my daily meal plan, I rotate fruits, vegetables, lean proteins like fish or poultry, nuts and seeds, legumes, whole grains such as oats or barley, low-fat or fat-free dairy, and healthy fats from olive oil and avocado.
The American Heart Association recommends limiting saturated fat, sodium, added sugar, red and processed meats, and avoiding trans fat, which can appear in some packaged baked goods and spreads. The DASH Diet earned the top ranking for heart health in 2025 because it emphasizes less sodium and more high-fiber foods, especially plants.
Current guidelines suggest limiting saturated fat to no more than 6 percent of calories to help prevent high LDL cholesterol, which raises the risk for coronary artery disease. I choose products with reduced sodium and pick nutrient-dense foods like sweet potatoes instead of white potatoes, or roasted chicken instead of fried options.
Key components of a heart-healthy diet
A heart-healthy diet focuses on foods that protect your circulatory system and improve cholesterol trends over time. I choose items rich in fiber, healthy fats, and vital nutrients to lower my risk of heart disease.
Which fruits and vegetables are best for heart health?
Leafy greens such as spinach and kale deliver fiber, potassium, and vitamins with very few calories. I usually include at least 2 cups of mixed salad greens with cherry tomatoes at dinner, which matches DASH-style meal ideas.
Bright vegetables like broccoli, cauliflower, bell peppers, and carrots are packed with antioxidants that help protect blood vessels. Eating 4 to 5 servings of fruits and vegetables each day matches National Heart, Lung, and Blood Institute guidance for a heart-healthy eating pattern.
Berries stand out. Blueberries and strawberries contain compounds linked to better cholesterol patterns. Bananas add potassium, which helps manage blood pressure by balancing the effects of sodium.
Peaches canned in juice make an easy snack without the added sugars found in many desserts. Kiwis offer vitamin C and a refreshing taste. I focus on colorful produce because it fills me up and leaves less room for salty snacks or sugary drinks.
Why focus on whole grains?
Whole grains support steady energy and heart protection. Oatmeal, brown rice, and whole-wheat pita offer fiber and nutrients that help lower LDL, the bad cholesterol.
I aim for 6 to 8 servings of grains per day on a 2,000 calorie DASH plan. A cup of cooked oats is my breakfast staple. It helps me stay full and supports healthy blood pressure.
Whole grains are low in saturated fat and supply vitamins, minerals, and antioxidants. They aid digestion and keep me satisfied longer than refined grains. Choosing brown rice or whole-wheat pita helps reduce two major risks for heart disease, high blood pressure and high LDL cholesterol.
How to reduce saturated and trans fats in your diet
Swap foods high in saturated and trans fats for healthier oils. I replace butter, lard, and tropical oils like coconut or palm with liquid vegetable oils such as canola, olive, soybean, corn, or sunflower oil.
I pick low-fat or fat-free dairy over whole milk, cheese, cream, and ice cream. The DASH plan favors lean proteins, so I choose skinless chicken breast, fish, or beans instead of fatty cuts of meat.
Processed foods often hide saturated or trans fats. I rely on the Nutrition Facts label to spot them in crackers, cookies, chips, and baked goods. On my sample menus, Day 1 has about 12 grams of saturated fat and Day 2 has roughly 11 grams. Almost no trans fat appears in either day.
What are the benefits of lowering sodium intake?
Low sodium eating helps keep blood pressure in a healthy range. The 2020 to 2025 Dietary Guidelines for Americans suggest no more than 2,300 mg of sodium per day. DASH shows even more benefit at 1,500 mg when possible.
High sodium intake raises the risk for heart disease and stroke. It can also damage arteries over time. I read labels to choose lower sodium foods, and I cook from scratch with herbs, citrus, and spices instead of salt.
My DASH-style sample days kept sodium to about 1,162 mg on Day 1 and 1,558 mg on Day 2. That made it easier to feel my best and stay consistent.
Which foods are rich in omega-3 fatty acids?
Fatty fish are top sources. Salmon, mackerel, sardines, tuna, and herring provide EPA and DHA, two omega-3 fats that support heart rhythm and healthy triglyceride levels. A 4 ounce salmon fillet appears in my Day 1 dinner.
Plant sources help too. Chia seeds, flaxseeds, walnuts, and canola oil contain ALA, a plant omega-3 fat. Regular intake supports lower triglycerides and better heart health.
How can you limit added sugars effectively?
I read ingredient lists and Nutrition Facts to find foods with less added sugar. I choose snacks, cereals, and yogurts marketed as no added sugar or low sugar. DASH suggests no more than five servings of sugary drinks and sweets per week.
On my sample menus, Day 1 includes about 6 grams of added sugar and Day 2 reaches 30 grams. I replace soda and sweet teas with water or unsweetened drinks. Fresh fruit doubles as dessert and cuts cravings.
High added sugar intake is linked to higher triglycerides and greater heart risk according to the American Heart Association. Keeping my meals close to whole foods helps me meet daily goals.
What are the benefits of a heart-healthy diet?
A heart-healthy diet boosts cardiovascular health, supports fitness, and guides daily choices. The benefits stack up over time.
How does it lower cholesterol levels?
Fiber from oats, beans, and leafy greens helps block some cholesterol absorption in the gut. Nuts, seeds, fish, and low-fat dairy provide protein and healthy fats that support lower LDL.
The DASH plan keeps saturated and trans fats low while adding key minerals like potassium and calcium. Roasting or grilling vegetables instead of frying reduces unhealthy oils. Trimming added sugar helps control triglycerides, which affect cholesterol patterns.
I also cook with olive or canola oil instead of butter. Watching sodium helps control blood pressure, which works together with cholesterol for better heart health.
How does it reduce blood pressure?
The DASH diet, rated the #1 Best Diet for High Blood Pressure in January 2025, lowers blood pressure with nutrient-rich foods and less sodium. It focuses on fruits, vegetables, whole grains, and lean proteins like beans and egg whites.
DASH recommends 1,500 to 2,300 milligrams of sodium per day. Lower sodium means less fluid retention so the heart pumps with less strain.
Switching from salty foods to fresh produce, unsalted nuts, and home-cooked recipes helps me keep my numbers in range. Many people see results within weeks.
How does it decrease the risk of heart disease?
Eating fewer saturated and trans fats, less sodium, and less added sugar can lower heart disease risk. I build meals around leafy greens, whole grains, omega-3 rich fish, and nuts.
Research shows replacing processed meats with plant proteins can reduce cardiovascular risk [1]. U.S. News & World Report ranked DASH the top Heart-Healthy Diet in 2025 because of outcomes like these.
Choosing low sodium foods supports healthy blood pressure. More fruits and vegetables add antioxidants that protect arteries. Each step reduces the chance of plaque buildup inside blood vessels, which lowers the risk of heart attack [2].
How does it help with weight management?
A heart-healthy diet plan helps me match calories in with calories out. It favors high fiber foods that keep me satisfied, such as greens, whole grains, beans, and fruit.
One serving of nuts or legumes gives protein without the saturated fats found in many processed meats. I swapped salty crackers for unsalted nuts and sliced vegetables. I felt fuller and reduced cravings.
Dietitians recommend at least 150 minutes of moderate exercise per week for weight control. Pairing movement with smart portions keeps my progress steady.
How does it improve overall cardiovascular health?
Weight control is only part of the picture. Foods rich in potassium, magnesium, calcium, fiber, and protein support healthy blood pressure and cholesterol together.
Leafy greens increase potassium, which helps counter sodium. Nuts supply unsaturated fats that support flexible arteries. Whole grains and legumes offer complex carbs for steady energy and better blood sugar control.
Well-studied patterns like Mediterranean and plant-forward diets show lower heart disease rates in many studies from Mayo Clinic and others. For best results, I also monitor my blood pressure at home and keep sodium in check.
Popular heart-healthy diet plans
Several plans use proven strategies to support heart health. I explored the most practical options and tried simple recipes first.
What is the DASH Diet and how does it work?
DASH stands for Dietary Approaches to Stop Hypertension. It lowers blood pressure by encouraging foods rich in potassium, calcium, magnesium, fiber, and protein while limiting sodium and saturated fat.
Daily goals include 6 to 8 servings of grains, fewer than 6 servings of lean meat, poultry, or fish, 4 to 5 servings each of fruits and vegetables, and 2 to 3 servings each of low-fat dairy and healthy oils. Weekly, I aim for 4 to 5 servings of nuts, seeds, or legumes and no more than five sweets.
No special foods are needed. Simple swaps, like whole grain crackers instead of salty snacks, make a big difference. Sodium stays under 2,300 mg per day. I build meals with legumes, leafy greens, and fruit, then layer in unsalted nuts for healthy fat.
The Mediterranean Diet shares many ideas with DASH, with a few unique touches worth noting next.
What are the principles of the Mediterranean Diet?
The Mediterranean Diet highlights olive oil, legumes, nuts, whole grains, fish like salmon or sardines, and plenty of fruits and vegetables. Dairy is moderate and red meat is limited.
People along the Mediterranean coast have eaten this way for decades. Studies associate their eating pattern with lower heart disease rates compared with many other regions.
A typical plate includes leafy greens or orange slices, a small handful of almonds or walnuts, grilled fish seasoned with herbs, and whole grain bread. Some adults choose a small glass of red wine with meals, although alcohol is optional and not safe for everyone.
These principles support heart health and are easy to blend with other plans. Plant-forward eating builds on the same ideas.
How do plant-based diets support heart health?
Plant-based diets rely on legumes, nuts, seeds, vegetables, fruits, and whole grains. These foods provide fiber and antioxidants that lower LDL cholesterol and support healthy arteries.
I often replace red meat with beans and lentils for protein. Studies from the American Heart Association show plant-focused eating can reduce heart disease risk by up to 32 percent.
Swapping crackers for a handful of walnuts or almonds helps manage cholesterol while curbing hunger. Plant-centric meals also tend to be lower in sodium, which supports healthy blood pressure.
Foods to include in your heart-healthy diet
I add a variety of nutrient-dense foods each week so meals stay interesting and support my goals. Simple choices create steady progress.
Why choose leafy greens and colorful vegetables?
Leafy greens like romaine and mixed salad greens appear in both DASH and my weekly plan. They deliver vitamins A, C, and K, plus folate and potassium.
I often mix two cups of salad greens with a half cup of cherry tomatoes for dinner. People who eat more leafy greens have lower cardiovascular risk in many studies.
Colorful vegetables guard the heart by reducing inflammation. Tomatoes offer lycopene and dark greens provide lutein, both helpful for vessel health. Eating at least 2.5 cups of vegetables per day supports better cholesterol patterns and lowers risk factors.
What fatty fish are best for your heart?
After adding greens, I reach for heart-healthy fish. Salmon tops my list for omega-3s that lower triglycerides and ease inflammation. A 4 ounce portion aligns with DASH guidance.
Sardines and mackerel offer similar benefits and often contain vitamin D. Tuna provides a lean protein option with less saturated fat than many red meats. I aim for two fish meals per week.
How do nuts and seeds benefit heart health?
I also include a variety of nuts and seeds. Almonds and sunflower seeds often go over green beans for crunch and nutrition. Regular portions of nuts can help lower LDL and calm inflammation related to heart risk.
DASH suggests four or five weekly servings of unsalted nuts, seeds, or legumes to support vessel health. Unsalted mixed nuts, my Day 2 snack, deliver protein, fiber, potassium, magnesium, and unsaturated fats that work together for heart health.
These nutrients help keep arteries flexible and may lower blood pressure. I often swap salty crackers for a small handful of raw or lightly toasted nuts.
…
^1 U.S. Department of Health & Human Services, Dietary Approaches to Stop Hypertension (DASH).
What role do legumes and beans play?
Legumes and beans act as budget-friendly protein and fiber sources without added saturated fat. DASH highlights them as smart replacements for red or processed meat.
A half cup serving can offer about 8 grams of protein and up to 7 grams of fiber. That supports healthy cholesterol and digestive health.
I add chickpeas or black beans to salads and soups, or mash them with avocado for a creamy dip that replaces salty, high fat spreads. Clinical research shows legume-rich diets can lower LDL cholesterol by about 5 percent over six weeks.
Lentils, kidney beans, peas, and pinto beans fit both Mediterranean and DASH patterns. These foods also provide potassium and magnesium, minerals linked with lower blood pressure.
Which whole grains are most heart-friendly?
Oatmeal is a standout for heart health. The soluble fiber beta-glucan helps lower LDL cholesterol. My weekly rotation also includes brown rice and whole-wheat pita.
Studies show three daily servings of whole grains can reduce cardiovascular disease risk by up to 22 percent. Quinoa and barley add vitamins, minerals, and antioxidants while keeping sodium low.
Whole-wheat bread or pita make good sandwich bases. I also switch to whole grain pasta to raise fiber. Corn tortillas are another simple upgrade with more nutrients than refined versions.
How do healthy fats like olive oil and avocado help?
Healthy fats from olive oil and avocado support heart health by replacing saturated fats with monounsaturated fats. Using liquid non-tropical oils instead of butter or stick margarine can lower LDL cholesterol.
The DASH plan encourages these swaps at every meal. Avocados add potassium, fiber, and antioxidants along with creamy texture. I add sliced avocado to salads or whole grain toast, then skip high sodium spreads.
Foods to limit or avoid
Some foods raise cholesterol or blood pressure more than you might expect. I keep an eye on these choices and plan simple swaps.
Why avoid processed and packaged foods?
Processed and packaged foods often contain extra sodium, saturated fat, trans fat, and added sugars. In the United States, most daily sodium comes from packaged foods, not from the salt shaker.
Too much sodium raises blood pressure, and diets high in saturated or trans fats can raise heart disease risk. Hydrogenated oils in baked goods and snack foods make matters worse.
I cook at home whenever I can so I control salt and fat. If I want a snack, I choose fresh fruit or vegetables instead of cookies or crackers.
What are the risks of high-sodium snacks?
High-sodium snacks raise blood pressure and strain the heart. Common foods like pizza, sandwiches, and soups can push sodium well past daily limits. Adults should aim for less than 2,300 milligrams per day.
I read labels and pick lower sodium versions. Too much salt can stiffen blood vessels and increase stroke risk over time. Steering away from salty snacks protects my heart and supports a better overall plan.
How do sugary beverages and desserts affect your heart?
Sugary drinks and desserts pack a lot of added sugar into small servings. Extra sugar adds calories without the nutrients your heart needs.
Limiting sugary drinks to five or fewer servings per week helped me steady my energy and manage cravings. High added sugar intake can raise triglycerides and strain the arteries, increasing long-term risk.
Why limit red and processed meats?
Red and processed meats often come with more saturated fat and sodium. Eating a lot of these foods can raise cholesterol and blood pressure, which increases heart disease risk.
DASH suggests choosing lean or unprocessed proteins such as skinless poultry or fish. I swapped bacon at breakfast for grilled chicken or beans and noticed a boost in energy.
What foods are high in saturated fats?
Fatty meats like bacon, sausage, and ribs are high in saturated fat. Full-fat dairy such as whole milk, cheese, cream, butter, and ice cream also add up fast.
Tropical oils like coconut and palm oil raise saturated fat quickly. Many packaged foods use these oils for texture. The DASH plan limits these items because higher saturated fat intake raises LDL cholesterol.
One tablespoon of coconut oil has about 12 grams of saturated fat. After reading labels and talking with my doctor, I swapped full-fat cheese for lower fat options.
Creating a balanced heart-healthy meal plan
I use a simple framework to keep meals balanced and portions right-sized. Planning ahead makes healthy habits easier.
How can you practice portion control?
Standard serving sizes keep portions in check. I follow DASH guidelines and aim for six to eight grain servings per day. I measure one cup of yogurt and four ounces of salmon, just like the sample menus.
Smaller plates help prevent overeating. I also portion snacks. A small bowl of nuts is better than eating from the bag. Reading labels shows me what counts as one serving.
What are easy meal prep ideas for busy schedules?
Quick staples work well on busy days. Oatmeal, yogurt with fruit, and whole-wheat pita sandwiches take less than 10 minutes. The Heart-Check mark from the American Heart Association helps me spot good options fast.
I batch cook grains like brown rice and quinoa on weekends. I pre-chop vegetables and portion unsalted nuts so I can build meals in minutes.
How do you balance macronutrients for heart health?
I include lean protein, whole grains, fruits, and vegetables at every meal. On Day 1, I reach around 1,688 calories, 46 grams of total fat, 94 grams of protein, and 242 grams of carbohydrates.
On Day 2, I target about 1,621 calories with 31 grams of total fat, 83 grams of protein, and 246 grams of carbohydrates. The aim is low saturated fat, high fiber, and strong nutrient density.
I prep meals ahead so portions stay on track. A palm-sized piece of chicken or fish at lunch or dinner sets my protein. Half my plate is colorful vegetables, and a small scoop of brown rice or quinoa rounds out the meal.
Sample 2-day heart-healthy meal plan
Here is a simple two-day plan you can adapt to your taste and budget. Use it as a starting point for your own routine.
What does a heart-healthy breakfast, lunch, dinner, and snacks look like on Day 1?
Breakfast: 1 cup cooked oatmeal topped with 1 tablespoon walnuts and 1 teaspoon cinnamon. Add a sliced banana and 1 cup skim milk for potassium and calcium.
Lunch: 1 cup low-fat plain yogurt mixed with 1 teaspoon ground flaxseed, 1 cup peach halves, and five Melba toast crackers. Raw broccoli and cauliflower with 2 tablespoons low-fat cream cheese on the side. Sparkling water to drink.
Dinner: 4 ounces salmon, 1/2 cup green beans with 1 tablespoon toasted almonds, and a salad with 2 cups greens, 1/2 cup cherry tomatoes, 2 tablespoons low-fat dressing, and 1 tablespoon sunflower seeds. A small orange and a glass of skim milk.
Snacks: 1 cup skim milk with 1/4 cup raisins or unsweetened dried fruit, plus 20 dark chocolate chips.
Daily totals: About 1,688 calories, 46 g total fat, 12 g saturated fat, 94 g protein, 242 g carbs, 29 g fiber, 1,162 mg sodium, 4,764 mg potassium, 1,700 mg calcium, plus magnesium and iron.
What does a heart-healthy breakfast, lunch, dinner, and snacks look like on Day 2?
Breakfast: 1 cup plain low-fat yogurt with blueberries, plus 3/4 cup calcium-fortified orange juice.
Lunch: Whole-wheat pita stuffed with shredded romaine, sliced tomatoes, cucumbers, and crumbled feta. Reduced-fat ranch dressing. A kiwi and 1 cup skim milk.
Dinner: 3 ounce chicken stir-fry with eggplant and basil, cooked with 1 tablespoon low-sodium teriyaki sauce. Brown rice topped with chopped dried apricots. A small glass of red wine or 4 ounces of 100 percent grape juice for polyphenols.
Snacks: 2 tablespoons mixed unsalted nuts and 1 cup fat-free frozen yogurt.
Daily totals: About 1,621 calories, 31 g total fat, 11 g saturated fat, 83 g protein, 246 g carbs, about 3,353 mg potassium. Portion control helps this plan fit busy schedules.
Tips for dining out on a heart-healthy diet
I look for heart-friendly choices on menus and ask simple questions. Small requests can cut a lot of sodium and saturated fat.
How to choose heart-friendly options at restaurants?
I check nutrition information online when possible. I look for dishes lower in sodium, added sugars, and saturated fat. The American Heart Association suggests less than 2,300 mg sodium daily for adults, and some meals exceed that in one plate.
I pick grilled chicken, steamed vegetables, or salads with oil and vinegar instead of creamy dressings. I ask for sauces on the side and choose baked or grilled items rather than fried.
How to avoid hidden sodium and unhealthy fats when dining out?
I scan for labels like low sodium or heart-healthy. I request light salt in the kitchen and ask for dressings on the side. Many dishes contain more than 2,300 mg sodium per serving.
Grilled options often contain less unhealthy fat than fried choices. I check nutrition pages for chains to compare plates. One time, a veggie stir-fry had nearly half a day of sodium from soy sauce, so I asked for less sauce and felt better after the meal.
Lifestyle tips to complement your diet
Habits beyond the plate matter too. Movement, sleep, and stress management help your heart work more efficiently.
How to incorporate regular exercise for heart health?
I aim for at least 150 minutes a week of moderate activity like brisk walking or cycling. Some weeks, I swap in 75 minutes of vigorous activity like jogging or swimming.
Short sessions count. Ten-minute walks after meals add up fast. I also take the stairs and walk during calls. Strength training two days a week supports heart health by adding muscle and improving metabolism.
Regular movement lowers blood pressure and improves mood. Even small steps, such as a short lunchtime walk, create progress over time.
What are effective ways to manage stress?
Daily walks and simple breathing exercises ease tension. Yoga or mindfulness can quiet my mind and improve sleep. Mayo Clinic resources on sleep and self-care tips have helped me build a routine.
I limit caffeine later in the day and keep a short gratitude list at night. Chronic stress can raise blood pressure and cholesterol, so I treat stress control like any other health habit.
Why is staying tobacco-free important?
Staying tobacco-free is vital for heart health. Smoking and nicotine products damage arteries and raise heart disease risk. The CDC reports smokers are two to four times more likely to develop coronary heart disease than non-smokers.
Benefits start quickly after quitting. The American Heart Association notes a drop in heart attack risk within 24 hours of stopping. Avoiding all forms of tobacco supports healthy cholesterol levels and stronger arteries.
How do you monitor progress and stay consistent?
I keep a simple meal and exercise journal. Tracking turned vague goals into clear steps that I can repeat each week.
What are the best ways to track your meals and health metrics?
I use tools like MyFitnessPal, Cronometer, or Lose It! to log foods and review my intake against DASH-style targets. Barcode scanners and large food databases make tracking easier.
Worksheets or spreadsheets help me monitor sodium, calories, fiber, and saturated fat. A 2022 American Heart Association review linked regular tracking with better diet adherence and improved outcomes.
Seeing weekly trends helped me spot high sodium days and low fruit intake. I then adjusted my grocery list and recipes.
When and how should you adjust your diet plan?
Life changes may require shifts in calories or activity. The American Heart Association suggests aligning intake and exercise with your age, sex, medical conditions, and goals.
If I gain weight despite regular movement, I reduce daily calories by 200 to 300 or add extra steps. If my blood pressure rises above 120 over 80 mmHg, I lower sodium by avoiding canned soups and salty snacks.
Tracking showed me that too much cheese raised my LDL cholesterol. Cutting back improved my next lab results. Small adjustments keep progress moving without feeling extreme.
Common myths about heart-healthy diets
Misconceptions can derail good intentions. Clearing them up makes it easier to choose foods with confidence.
What misconceptions exist about fats and cholesterol?
Not all fats are harmful. Saturated and trans fats raise LDL cholesterol and heart risk, especially in fried snacks, processed meats, and packaged baked goods. In contrast, monounsaturated and polyunsaturated fats in olive oil, avocados, nuts, and fatty fish can lower LDL and support HDL, the good cholesterol.
Another myth says dietary cholesterol always raises blood cholesterol. Research shows saturated fat has a stronger effect than foods like eggs or shellfish for most people. I switched from butter to olive oil and saw better lipid results during my next checkup.
What is the true role of carbohydrates in heart health?
Carbohydrates help or harm depending on the source. Whole grains and nutrient-dense carbs add fiber, vitamins, and minerals that support healthy pressure and cholesterol.
Oats, quinoa, brown rice, barley, and sweet potatoes deliver steady energy without sharp spikes in blood sugar. Refined carbs, like white bread and sugary snacks, increase triglycerides and weight gain risk.
Research links whole grain intake with lower cardiovascular disease risk. I now choose steel-cut oats over processed cereal, and my morning energy lasts longer.
Conclusion
A heart-healthy diet, such as a DASH-style plan rich in whole grains, fruits, vegetables, healthy fats, and lean proteins, helps lower cholesterol and blood pressure. Cutting sodium and added sugars reduces the risk of heart disease.
Even small steps lead to meaningful gains in heart health, according to the American Heart Association. Talk with a healthcare professional if you have medical conditions or take medications, especially for blood pressure or cholesterol. I focus on one change at a time, then build from there for lasting results.
FAQs
1. What foods should I include in a heart healthy diet plan?
A heart healthy eating plan includes plenty of vegetables, fruits, whole grains such as brown rice and oats, lean proteins like fish or poultry, legumes such as beans and lentils, nuts, seeds, and low-fat dairy products. Studies show that diets rich in these foods can lower cholesterol and blood pressure levels (American Heart Association).
2. How much sodium is recommended for better heart health?
Experts recommend limiting sodium to less than 2,300 milligrams per day for most adults; some groups may benefit from even lower intake. High sodium consumption raises the risk of high blood pressure according to research published by the Centers for Disease Control and Prevention.
3. Can following this eating plan help reduce my risk of cardiovascular disease?
Yes; evidence supports that a balanced meal pattern with reduced saturated fat and added sugars lowers the chance of developing cardiovascular conditions. For example, one large study found people who followed a Mediterranean-style diet had up to 30 percent fewer cardiac events compared to those on standard diets (New England Journal of Medicine).
4. How do I start making changes toward a healthier meal routine?
Begin by adding more plant-based options at each meal; swap refined grains for whole versions like quinoa or barley; choose grilled instead of fried meats; use herbs rather than salt for flavoring food. When I started preparing meals ahead using these tips it became easier to stick with nutritious choices throughout busy weeks.
Summary: A well-structured heart healthy eating plan focuses on nutrient-rich ingredients while reducing salt and unhealthy fats. Research shows consistent habits support long-term wellness outcomes including improved cholesterol numbers and reduced disease risks.







