Pregnancy Diet Plan: Healthy Eating For Expecting Moms
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
If you feel unsure about what to eat during pregnancy, you are not alone. A simple pregnancy diet helps you meet your needs and your baby’s needs at the same time. Many women fall short on key vitamins and minerals, which can affect health during pregnancy. This guide offers practical meal ideas, proven nutrients, and easy tips to build a healthy diet.
You will learn how nutrition during pregnancy supports growth, protects your health, and fits into daily life. Use these ideas to plan meals, shop smarter, and feel confident at every stage.
Key Takeaways
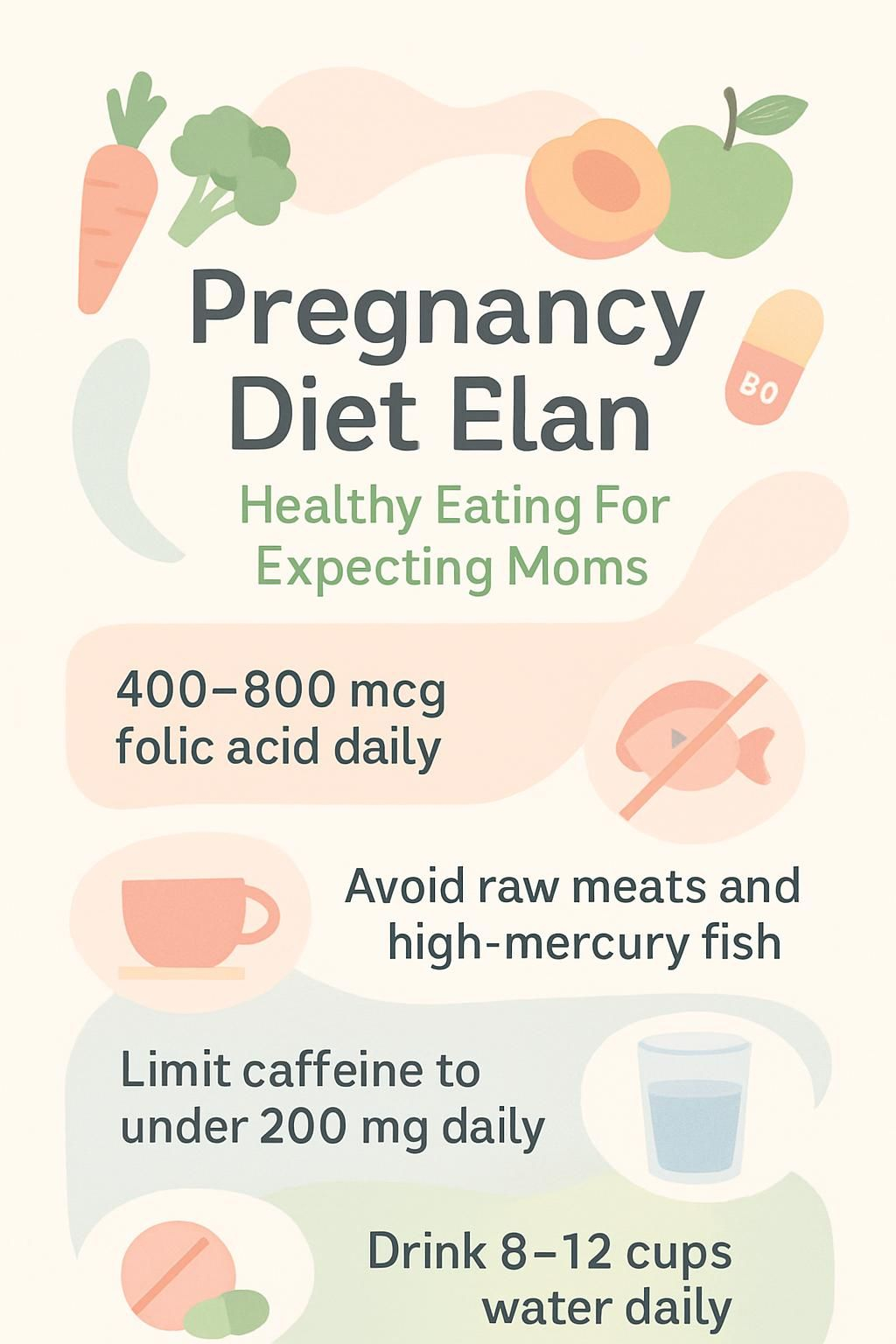
- Most expecting moms need 400 to 800 micrograms folic acid, 27 milligrams iron, 1,000 milligrams calcium, and 600 IU vitamin D daily (ACOG, CDC).
- Avoid raw or undercooked meats, high-mercury fish like shark or king mackerel, unpasteurized cheeses, and keep caffeine under 200 milligrams per day.
- A balanced plate with fruits, vegetables, lean protein, whole grains, fiber, and healthy fats supports fetal growth and lowers pregnancy risks.
- Drink 8 to 12 cups of water daily to prevent constipation and support healthy amniotic fluid levels (CDC).
- Prenatal vitamins fill gaps, but they do not replace a varied, nutrient-rich diet.
Why Is Nutrition Important During Pregnancy?

What you eat shapes your health and your baby’s development. Good nutrition during pregnancy covers growth, brain development, and your strength for the months ahead.
How does nutrition support fetal growth and development?
Your daily meals deliver the building blocks your baby needs. Folic acid, iron, calcium, protein, omega-3s, vitamin D, iodine, and choline support brain, spine, blood, and bone development. Folic acid lowers the risk of neural tube defects like spina bifida.
A nutrient-dense pattern also supports a healthy birth weight and lowers the risk of preterm delivery. Choose leafy greens, dairy or fortified milk for calcium, beans and lean meat for iron, eggs for choline, salmon for omega-3s, whole grains for energy, and fruit for fiber. Small, steady improvements add up over time.
How does nutrition promote maternal health?
A balanced diet strengthens your immune system and supports blood production. Iron helps prevent anemia, which can cause fatigue and affect oxygen delivery to the baby. Calcium supports bone strength, nerves, and a steady heart rhythm.
Fiber keeps digestion regular and eases constipation, which is common in pregnancy. Healthy fats from fish, nuts, and seeds provide energy and support cell health. Eating well also supports steady weight gain, which can reduce the risk of high blood pressure and gestational diabetes.
How can proper nutrition reduce the risk of birth defects?
Folic acid before pregnancy and during the first trimester helps prevent neural tube defects. Aim for at least 400 micrograms daily from fortified cereal, leafy greens, beans, and a prenatal vitamin. Vitamin B12 supports the brain and spine. Iron helps red blood cells carry oxygen to your baby.
Avoid high-risk foods such as unpasteurized cheese, raw or undercooked eggs, and seafood high in mercury like shark or bigeye tuna. Build most meals from whole foods, including whole grains, fruits, vegetables, lean protein, and dairy or fortified milk to cover the essential nutrient needs of prenatal development.
Essential Nutrients for Expecting Moms
Your body needs extra nutrients to support pregnancy and breastfeeding. These core nutrients help your baby grow and keep you healthy throughout pregnancy.
Why is folic acid important during pregnancy?
Folic acid, also called folate when found in foods, supports the baby’s brain and spinal cord. Taken before pregnancy and during the first trimester, it lowers the risk of neural tube defects.
Experts recommend 400 to 800 micrograms daily if you may become pregnant or are pregnant. You can find folate in fortified cereal, leafy greens, beans, eggs, and orange juice. Most diets fall short, so a prenatal vitamin helps you meet the target every day.
How does iron benefit pregnant women?
Iron helps your body make hemoglobin, the protein in red blood cells that carries oxygen. During pregnancy, your blood volume rises by about 50 percent. This increase raises your need for iron.
Low iron can cause tiredness and dizziness. It can also raise the risk of early delivery. Aim for 27 milligrams per day from food or a supplement during pregnancy. Good sources include lean red meat, beans, lentils, spinach, peas, fortified cereal, and eggs. Adding vitamin C foods, like oranges or tomatoes, improves iron absorption from plant sources. Ask your healthcare provider about a blood test if you think your levels are low.
What role does calcium play in pregnancy?
Calcium builds your baby’s bones and teeth, and it supports your muscles, nerves, and heartbeat. Aim for 1,000 milligrams every day. If intake is low, your body will pull calcium from your bones.
Choose dairy like milk and yogurt, or fortified options such as calcium-set tofu and fortified orange juice. Leafy greens like kale and broccoli also help. Adequate calcium may reduce the risk of high blood pressure in pregnancy.
How much protein do expecting moms need?
You need more protein to build your baby’s tissues and organs. Target about 71 grams per day during pregnancy. Mix animal and plant sources to meet your goal.
Include lean meats, eggs, tofu, beans, nuts, dairy, and lentils. If you are vegetarian, pair foods like beans and rice to cover all essential amino acids. Planning your meals helps you hit your daily target without stress.
Why are omega-3 fatty acids crucial during pregnancy?
Omega-3 fatty acids, especially DHA, support brain and eye development. They may lower the risk of early birth and support a healthy pregnancy weight. DHA builds cell membranes in the fetal brain and retina.
Salmon, sardines, walnuts, chia seeds, and fortified eggs are strong options. Many professionals suggest 200 to 300 milligrams of DHA daily. If you do not eat fish, ask your provider about a prenatal omega-3 supplement.
How does vitamin D support pregnancy health?
Vitamin D helps you absorb calcium and supports immune function. Low levels are common in pregnancy and may be linked to low birth weight or preeclampsia. Aim for 600 IU each day.
Sources include fortified milk, fortified orange juice, and cereals. Safe sun exposure helps too. Your provider may suggest a supplement if your levels are low.
What is the importance of fiber for pregnant women?
Fiber eases constipation and keeps digestion regular. It also helps manage blood sugar and supports a healthy weight. Most pregnant women need 25 to 30 grams per day.
Choose whole grains, leafy vegetables, beans, lentils, berries, and citrus fruit. Even small changes, like adding oatmeal or a side salad, can make a difference in comfort and regularity.
Best Foods to Include in a Pregnancy Diet
A healthy diet is an important part of a healthy lifestyle during pregnancy. Simple, steady choices help you cover the nutrients you need for growth and energy.
What fruits and vegetables should pregnant women eat?
Colorful produce covers many vitamins, minerals, and fiber. Mix cooked and raw options to broaden variety and reduce boredom.
- Dark leafy greens like spinach and kale for folate, iron, and calcium.
- Citrus fruits like oranges and grapefruit for folate and vitamin C.
- Berries for vitamin C and antioxidants that support tissue health.
- Carrots and sweet potatoes for vitamin A, which supports eye development.
- Bananas and avocados for potassium to help ease muscle cramps.
- Broccoli and bell peppers for fiber that supports digestion.
- Apples or pears with the skin for steady blood sugar and fiber.
- Cooked tomatoes for lycopene, an antioxidant with protective effects.
- Wash produce well to lower the risk of foodborne illness like toxoplasmosis.
- Rotate your choices each week to cover a wide range of nutrients.
Which whole grains are best for expecting moms?
Whole grains offer fiber, B vitamins, and steady energy. They support digestion and help you feel full between meals.
- Oats for beta-glucan fiber, B vitamins, and iron.
- Brown rice for magnesium, selenium, and slow-digesting carbs.
- Quinoa for complete protein and extra minerals.
- Whole wheat bread for more fiber and folate than white bread.
- Barley for soluble and insoluble fiber to ease constipation.
- Millet for a gluten-free option rich in magnesium.
- Plain popcorn for a high-fiber, lower calorie snack.
A simple bowl of oatmeal with orange slices adds fiber and vitamin C without added sugar. It is a quick breakfast on busy mornings.
What are good sources of lean protein during pregnancy?
Lean protein supports tissue growth for you and your baby. Include a variety of well-cooked options to lower the risk of illness.
- Skinless chicken or turkey for high-quality protein with less fat.
- Fully cooked eggs for protein and choline. Avoid runny yolks.
- Low-mercury fish like salmon and tilapia. Skip undercooked seafood.
- Low-fat dairy such as Greek yogurt, cottage cheese, and pasteurized cheese.
- Lean cuts of beef or pork, cooked to a safe internal temperature.
- Beans, lentils, and soybeans for plant protein and fiber.
- Unsalted nuts and seeds for protein and healthy fats.
- Tofu or tempeh for versatile plant protein in stir-fries or bowls.
- Nut butters on whole grain toast or blended in smoothies.
- Fortified soy milk if you avoid dairy, to help meet protein needs.
Use separate cutting boards for raw meat and produce, and cook foods to safe temperatures to reduce infection risk.
Which healthy fats are safe to eat while pregnant?
Healthy fats support your baby’s brain and nervous system. They also help you absorb fat-soluble vitamins like A, D, E, and K.
- Avocados for monounsaturated fats. Add slices to salads and sandwiches.
- Olive or canola oil instead of butter for heart-healthy fats in cooking.
- Unsalted nuts, such as almonds or walnuts, for plant-based omega-3s.
- Seeds like chia and flax for fiber and omega-3s in yogurt or oatmeal.
- Fatty fish like salmon or sardines twice a week for DHA. Avoid high-mercury fish.
- Natural nut butters without added sugar or hydrogenated oils.
- Pasteurized milk and dairy for calcium and quality fats.
Swapping chips for avocado over whole grain pasta can satisfy cravings and provide steady energy in the afternoon.
What calcium-rich foods should be included in a pregnancy diet?
Calcium supports your baby’s bones and teeth, and keeps yours strong. Most pregnant women need about 1,000 milligrams per day.
- Low-fat milk or fortified plant milk, about 300 milligrams per cup.
- Yogurt, often over 250 milligrams per serving.
- Cheese like Swiss or cheddar, around 200 milligrams per ounce.
- Leafy greens such as kale and bok choy for absorbable calcium.
- Canned salmon with bones for calcium and protein.
- Calcium-set tofu, often up to 250 milligrams per half cup.
- Almonds for a smaller boost of calcium plus healthy fats.
- Fortified foods like some cereals and orange juice.
- Avoid soft cheeses like Brie and Camembert unless labeled pasteurized.
An afternoon yogurt can lift energy and help you reach your calcium target. Talk to your healthcare professional before making big changes to your food and drink plan.
What Foods Should Pregnant Women Avoid or Limit?
Some foods raise the risk of illness or exposure to toxins. Limiting these items helps protect both you and your baby.
Why avoid raw or undercooked meat and seafood?
Raw or undercooked meat and seafood can carry harmful bacteria like Salmonella and E. coli, or parasites such as Listeria and Toxoplasma gondii. Infections can be more severe during pregnancy and may lead to serious complications.
Fully cooking meat and seafood lowers these risks. Choose sushi made with cooked seafood or vegetarian options. Also check local fish advisories for safety guidance.
Which fish have high mercury levels to avoid?
Shark, swordfish, king mackerel, and tilefish contain high mercury levels. Tuna steak often contains more mercury than canned light tuna. Limit tuna steak and albacore, and prefer canned light tuna when you want tuna.
Safer choices include salmon, catfish, tilapia, pollock, shrimp, cod, and canned light tuna. These options provide protein and omega-3s with less mercury exposure.
Why should raw eggs be limited during pregnancy?
Raw or undercooked eggs can carry Salmonella, which may cause vomiting, diarrhea, and fever. Pregnant women are more vulnerable to dehydration and complications.
Avoid items made with raw eggs, like some homemade mayonnaise, hollandaise, raw batter, and some restaurant dressings. Choose fully cooked eggs or pasteurized egg products instead.
How do processed foods impact pregnancy health?
Many processed foods are high in sugar, sodium, and unhealthy fats. Frequent intake raises the risk of excess weight gain, high blood pressure, and gestational diabetes.
Processed meats may also contain preservatives like nitrates. Build most meals from whole foods to support steady energy and a healthy weight. Whole grains and fiber-rich sides give better fuel than white flour snacks and sweets.
Why is alcohol harmful during pregnancy?
Alcohol crosses the placenta and reaches your baby. Even small amounts can affect brain development and growth. Drinking during pregnancy may cause fetal alcohol spectrum disorders.
Experts advise avoiding all alcoholic drinks for the entire pregnancy. Choose sparkling water with fruit or a mocktail when you want a special drink.
How much caffeine is safe for expecting moms?
Limit caffeine to about 200 milligrams per day. This equals roughly one 12-ounce cup of coffee or two cups of tea. Caffeine can cross the placenta and may affect heart rate and growth.
Read labels on soda, chocolate, and energy drinks. Switching to decaf or caffeine-free herbal tea in the afternoon may improve sleep and reduce jitters.
Typical Caffeine Content in Common Foods
| Item | Amount (mg) |
|---|---|
| Coffee, 8 oz | 80–100 |
| Tea, 8 oz | 30–50 |
| Chocolate bar, 1 oz | 10–20 |
| Soda, 12 oz | 30–40 |
Use these numbers to track your daily total as part of a healthy diet during pregnancy.
Sample Pregnancy Meal Plan
A simple pregnancy meal plan helps you cover key nutrients without guesswork. Mix and match options to fit your tastes, schedule, and budget.
What is a healthy breakfast for pregnant women?
Build breakfast with protein, fiber, healthy fats, and complex carbs. Try scrambled eggs with whole grain toast and sliced avocado. Add a glass of low-fat milk or fortified orange juice for calcium and vitamin D.
Oatmeal cooked with milk and topped with walnuts or ground flax gives fiber and omega-3s. Greek yogurt with nuts, chia seeds, and fruit adds protein and probiotics.
Sample Macronutrient Breakdown for a Healthy Breakfast
| Food Choice | Protein (g) | Fiber (g) | Iron (mg) | Calcium (mg) |
|---|---|---|---|---|
| 2 eggs | 12 | 0 | 2.0 | 60 |
| Whole grain toast | 4 | 3 | 1.0 | 40 |
| Avocado, half | 2 | 5 | 0.6 | 10 |
| Low-fat milk, 8 oz | 8 | 0 | 0.1 | 300 |
| Mixed berries, 1/2 cup | 0.5 | 2 | 0.3 | N/A |
Pair plant iron, such as spinach in an omelet, with vitamin C foods like peppers or oranges to boost absorption.
What should pregnant women eat for lunch?
Build lunch with lean protein, whole grains, colorful produce, and a calcium source. Try grilled chicken on whole wheat bread, a spinach and tomato side salad, and low-fat yogurt.
Beans or lentils give plant protein and extra fiber. Use pasteurized dairy and avoid processed meats unless heated until steaming. Grain bowls with salmon and broccoli deliver omega-3s and nutrients without feeling heavy.
What are nutritious dinner options during pregnancy?
Grilled salmon with quinoa and steamed broccoli offers protein, omega-3s, and fiber. Black bean tacos with avocado, tomatoes, and lettuce supply iron and healthy fats.
Chicken stir-fry with brown rice, bell peppers, and snap peas is rich in vitamin C and folate. Lentil soup with whole wheat bread supports protein and fiber needs. A baked sweet potato topped with cottage cheese or sautéed spinach gives calcium and vitamin A.
What are healthy snack ideas for expecting moms?
Choose snacks that add protein, fiber, and healthy fats. These help manage hunger between meals and stabilize energy.
- Greek yogurt with fresh fruit for protein, calcium, and vitamin C.
- Apple slices or whole grain toast with peanut or almond butter.
- Hummus with carrot sticks or bell pepper strips.
- Trail mix with unsalted nuts, seeds, and a little dried fruit.
- Cottage cheese with sliced peaches or pineapple.
- Hard-boiled eggs with whole wheat crackers for choline and fiber.
Additional Tips for Healthy Eating During Pregnancy
Small tweaks can improve comfort, energy, and digestion. These habits make healthy eating easier to maintain throughout pregnancy.
How much water should pregnant women drink daily?
Aim for 8 to 12 cups of water daily, about 64 to 96 ounces. Your body needs more fluids as blood volume increases.
Water transports nutrients to your baby, supports digestion, and helps prevent constipation. It also supports amniotic fluid and may lower the risk of urinary tract infections. Carry a water bottle, and add lemon or cucumber if you want flavor.
Why take a prenatal vitamin every day?
A daily prenatal vitamin supports gaps that food may not fill, especially during nausea or busy weeks. It should include folic acid, iron, vitamin D, and other essentials for pregnancy nutrition.
Taking at least 400 micrograms of folic acid from a prenatal vitamin before conception and in early pregnancy can reduce neural tube defects. Use it as a safety net, not a replacement for a balanced diet.
Why avoid fad diets and extreme restrictions during pregnancy?
Fad diets often cut whole food groups. That can lead to low energy and missed nutrients that you and your baby need. Restrictive plans can also raise the risk of poor outcomes.
Focus on variety from all food groups, including fruits, vegetables, whole grains, lean protein, healthy fats, and calcium-rich foods. Balanced meals support steady weight gain and consistent energy.
When should you consult a healthcare professional about your diet?
Contact your healthcare professional if you have severe nausea, rapid weight changes, or trouble keeping food down. Seek care if you develop new food allergies or follow a strict vegetarian or vegan diet and worry about nutrients.
If you have diabetes, high blood pressure, or digestive disease, ask for a referral to a registered dietitian who specializes in prenatal care. Discuss any supplement during pregnancy to avoid interactions. Call your provider for symptoms like rapid heartbeat, swelling, or hives after eating.
How Can Diet Help Manage Common Pregnancy Challenges?
Smart food choices can ease common concerns like nausea, constipation, and weight gain. A few small changes go a long way.
How to address morning sickness with food?
Eat small, frequent meals and snacks. Keep crackers near your bed and nibble before getting up. Choose bland foods like rice, bananas, potatoes, and applesauce.
Cold foods and simple flavors are often easier to tolerate. Sip water, clear broth, or diluted juice between meals. Ginger tea or ginger chews may also help some people.
What foods help prevent constipation in pregnancy?
Increase fiber and fluids. Choose oatmeal, whole wheat bread, brown rice, beans, lentils, broccoli, carrots, spinach, and sweet potatoes. These foods add bulk and support regularity.
Drink water throughout the day to help fiber do its job. If you like smoked foods as a cooking style, keep added fats light so digestion stays comfortable.
How to manage healthy weight gain through portion control?
Use smaller plates and bowls to guide portions. Fill half your plate with vegetables, a quarter with lean protein, and the last quarter with whole grains.
Eat slowly and pause to notice fullness. Pre-portion snacks instead of eating from the package. Track serving sizes with measuring cups, and choose water or milk over sweetened drinks.
Nutrition Needs During Each Trimester
Each trimester brings new needs for growth and energy. Focus on a few key nutrients at every stage to stay on track.
What should you focus on in the first trimester?
Folic acid is the top priority in early pregnancy. Aim for 400 to 800 micrograms per day, starting before conception and continuing through at least week twelve.
Add iron-rich foods like lean meat, beans, and fortified cereal to support rising blood volume. Drink plenty of water. Small, frequent meals with whole grains, fruits, and vegetables can ease queasiness and keep energy steady. Use a prenatal vitamin as recommended by your provider.
How do iron and calcium needs change in the second trimester?
Iron needs remain high as your blood volume expands. Keep aiming for 27 milligrams daily. Red meat, spinach, lentils, and fortified cereal are helpful sources.
Calcium needs stay at about 1,000 milligrams per day, and absorption improves mid-pregnancy. Add dairy, leafy greens, tofu, or fortified juices. Pair iron-rich meals with vitamin C foods like oranges or bell peppers to enhance absorption.
What nutrients are important in the third trimester?
Growth speeds up in the third trimester. You still need about 71 grams of protein and 27 milligrams of iron daily. Add omega-3s for brain development with foods like salmon and chia seeds.
Calcium remains essential at 1,000 milligrams per day, along with vitamin D for absorption. Aim for at least 28 grams of fiber to ease constipation. Whole grains, fruits, vegetables, nuts, and seeds help you meet this goal while keeping energy stable.
Meeting these targets supports healthy delivery outcomes and lowers risks like preterm birth or low birth weight, as noted by ACOG.
How Can Vegetarians and Vegans Maintain a Healthy Pregnancy Diet?
Plant-based eating can fully support a healthy pregnancy with planning. Focus on protein, calcium, iron, vitamin B12, iodine, and omega-3s from reliable sources.
What are good plant-based protein and calcium sources?
- Tofu, tempeh, and edamame for protein with some calcium.
- Beans, lentils, and chickpeas with 7 to 9 grams of protein per half cup.
- Fortified soy or almond milk, often 300 milligrams of calcium per cup.
- Almonds, chia, and sesame seeds for healthy fats and minerals. Two tablespoons of chia offer a notable calcium boost.
- Leafy greens like kale, bok choy, and collards for absorbable calcium.
- Hummus as a protein-rich spread or dip at lunch or snack time.
- Nutritional yeast, if fortified, for protein and added B12.
Add greens to smoothies or soups if you prefer milder flavors. Small swaps make plant-forward eating easier to maintain.
Which fortified foods provide vitamin B12 and iron?
- Breakfast cereals fortified with both vitamin B12 and iron. Check labels for amounts per serving.
- Fortified plant milks that add vitamin B12 and sometimes iron. Pour into oatmeal or smoothies.
- Nutritional yeast fortified with B12 for a cheesy flavor on pasta or vegetables.
- Some meat alternatives like veggie burgers or tofu products with added B12 and iron.
- Energy bars made for prenatal needs that include B12 and iron. Use for on-the-go snacks.
- Whole grain breads that list added B12 or iron on the nutrition panel.
These foods help you meet targets without relying only on supplements. Ask your provider if you should add a B12 tablet or an iron supplement.
Conclusion
A thoughtful pregnancy diet supports your health and your baby’s growth. Build most meals from fruits, vegetables, lean proteins, whole grains, fiber, and healthy fats. Limit high-mercury seafood, unpasteurized cheese, and undercooked animal foods. Keep caffeine modest and avoid alcohol.
Drink plenty of water and take a prenatal vitamin daily to cover common gaps. If you have questions about your pregnancy meal plan or specific needs, talk to your healthcare professional or a registered dietitian. This guide is educational and does not replace medical advice.
References:
- American College of Obstetricians and Gynecologists (ACOG). “Nutrition During Pregnancy.”
- Centers for Disease Control and Prevention (CDC). “Pregnancy Nutrition Facts.”
FAQs
1. What foods should expecting mothers include in a pregnancy diet plan?
Expecting mothers benefit from eating whole grains, lean meats, dairy products like yogurt and cheese, fresh fruits such as oranges and berries, leafy greens including spinach and kale, beans, nuts, and seeds. These foods provide protein, calcium, iron, folic acid, fiber, vitamin C, and healthy fats that support fetal growth according to the American College of Obstetricians and Gynecologists.
2. How much weight gain is considered healthy during pregnancy?
The Centers for Disease Control recommends most women with a normal pre-pregnancy weight gain between 25 to 35 pounds throughout pregnancy. Women carrying twins or those underweight before conception may need more; those overweight may require less. Regular checkups help track progress.
3. Are there specific nutrients that are especially important for pregnant women?
Pregnant women need extra folic acid to prevent neural tube defects; iron supports increased blood volume; calcium strengthens bones; omega-3 fatty acids aid brain development; vitamin D helps absorb calcium efficiently. A registered dietitian can offer guidance on meeting these needs through food choices or supplements if necessary.
4. Can you share an example of how a balanced meal looks for an expecting mother?
A typical lunch might feature grilled chicken breast served over brown rice with steamed broccoli plus sliced strawberries on the side along with low-fat milk or fortified orange juice. This combination supplies protein for tissue growth as well as vitamins A and C plus minerals vital for both mother’s health and baby’s development.
Summary: Expecting mothers should focus on nutrient-rich meals containing proteins like poultry or fish paired with vegetables such as broccoli or spinach alongside whole grains like brown rice plus fruit options including berries or citrus while monitoring weight changes under medical supervision to ensure optimal outcomes for themselves and their babies.







