Losing Weight While Pregnant: Effective Strategies For Safe Pregnancy Weight Loss
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
If you feel nervous about weight changes in pregnancy, you are in good company. Many people begin pregnancy overweight or with obesity, and the topic can feel complicated. You may ask if it is safe to lose weight while pregnant, or how much gain supports your baby best.
This guide uses trusted sources, including the Centers for Disease Control and Prevention, to explain safe, realistic steps. You will learn what weight loss during pregnancy means, how to protect fetal growth, and when to call your care team. Use these tips to support a healthy pregnancy with confidence.
Key Takeaways
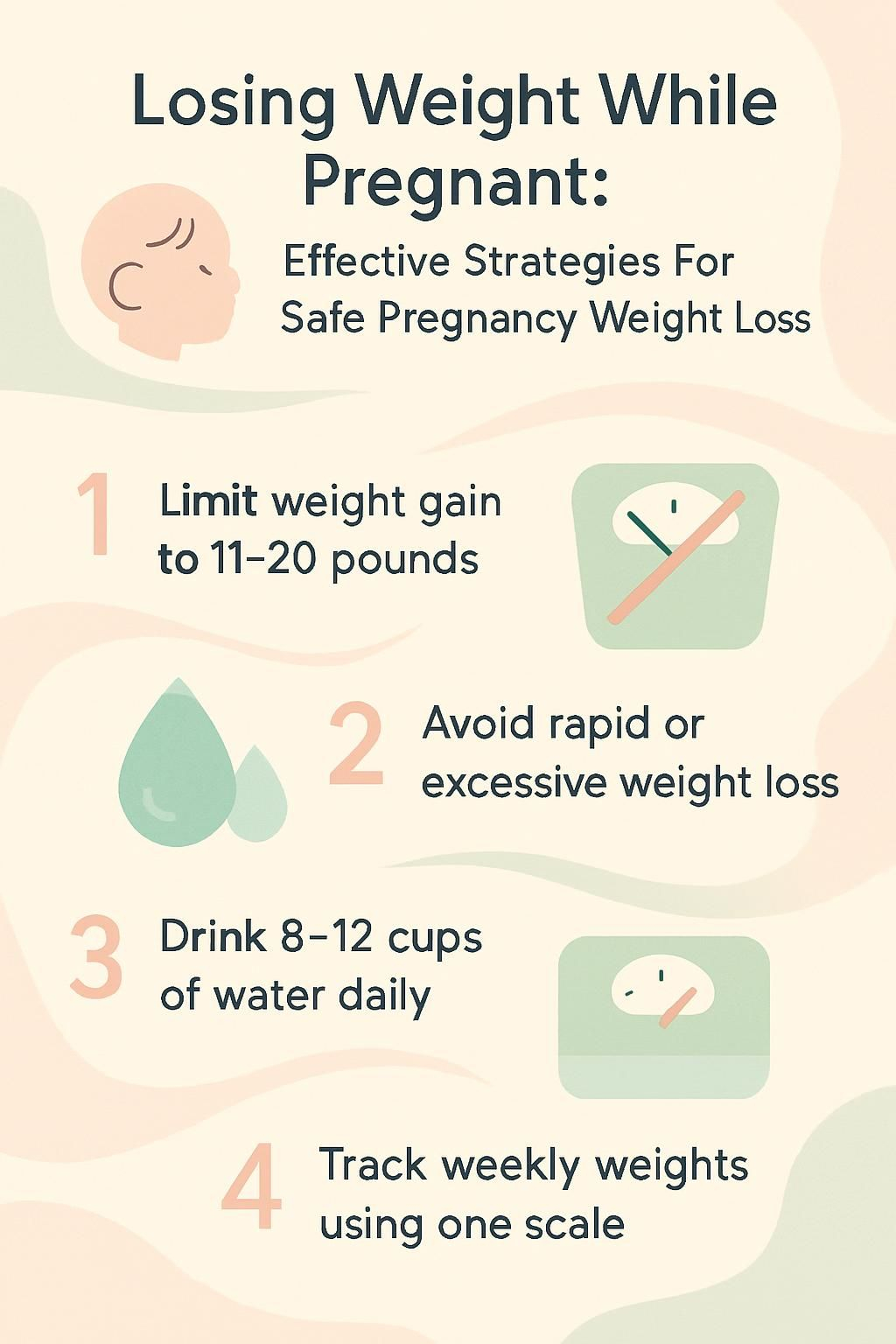
- Experts, including the CDC, advise those with a pre-pregnancy BMI of 30 or higher to limit total pregnancy weight gain to 11 to 20 pounds.
- Rapid or large weight loss can raise the risk of low birth weight, malnutrition, and problems such as neural tube defects. Seek urgent care for severe fatigue, dehydration, or reduced fetal movement.
- Protect yourself by checking with your OBGYN before diet changes, choosing nutrient-dense foods like lean protein and whole grains, and drinking 8 to 12 cups of water daily.
- Moderate exercise, such as walking, swimming, prenatal yoga, and light strength work, helps manage weight safely. Always get medical clearance first.
- Track weight weekly on the same scale at home. Adjust food and activity with professional guidance to support both you and your baby.
Understanding Weight Loss Safety During Pregnancy

Knowing what is safe helps you care for yourself and your baby. Before you try to change weight during pregnancy, learn how weight shifts usually occur and what warning signs matter.
What are the risks of losing weight while pregnant?
Unplanned weight loss can strain your baby’s growth. It raises the chance of low birth weight, which connects to breathing, feeding, and learning concerns later in life.
Losing 5 to 10 percent of your body weight may point to hyperemesis gravidarum, a severe form of morning sickness. This condition can cause dehydration, fewer bathroom trips, and electrolyte problems. It needs quick care.
Too few calories or vitamins can also reduce nutrients for prenatal development. That can increase the risk of neural tube defects if folate and other key nutrients are low. Sudden drops in maternal weight often signal trouble, even when conditions like gestational diabetes are being treated.
Call your provider right away if weight falls quickly and you also notice strong fatigue, dizziness, or less fetal movement.
If weight drops too much in pregnancy, both your health and your baby’s well-being can be at risk.
When is weight loss recommended during pregnancy?
Doctors may discuss limited weight gain or careful weight reduction if you begin pregnancy with obesity, defined as a BMI of 30 or higher. This is especially true with a BMI above 40, where risks such as preeclampsia, hypertension, and delivery complications increase.
The CDC suggests a total gain of 11 to 20 pounds for a BMI of 30 or more. Some high-risk cases may focus on weight maintenance or a very slight loss, always under close medical supervision.
Any plan should include frequent checks of fetal growth, usually with ultrasounds and regular prenatal visits. Your team will follow evidence-based guidance from obstetrics and gynecology groups.
Do not diet on your own. Speak with your OBGYN before changing food or activity. Restricting important nutrients can harm fetal growth.
Healthy Weight Management Guidelines in Pregnancy
Healthy weight management supports your baby’s growth and lowers chances of problems. Clear targets for each trimester make daily choices easier.
Why is maintaining weight balance important in pregnancy?
Gaining too much weight can raise your risk of high blood pressure, preeclampsia, gestational diabetes, and the need for a cesarean delivery. Babies also face a higher chance of preterm birth and breathing issues.
On the other side, gaining too little can threaten fetal growth. Most development speeds up in the second and third trimesters. Many people gain 1 to 4 pounds in the first trimester, then about a pound per week after that, depending on BMI.
Experts agree that staying within a healthy range supports better outcomes for both mother and infant.
How much weight should I gain each trimester?
Target ranges help you plan meals and activity with confidence. The table below summarizes CDC guidance for total gain and weekly pace by pre-pregnancy BMI.
| Pre-Pregnancy BMI | Category | Total Recommended Weight Gain | 1st Trimester (Weeks 1–12) | 2nd Trimester (Weeks 13–26) | 3rd Trimester (Weeks 27–Birth) |
|---|---|---|---|---|---|
| <18.5 | Underweight | 28–40 lbs | 1–5 lbs | ~1 lb/week | ~1 lb/week |
| 18.5–24.9 | Normal weight | 25–35 lbs | 1–5 lbs | ~1 lb/week | ~1 lb/week |
| 25.0–29.9 | Overweight | 15–25 lbs | 1–5 lbs | ~0.6 lbs/week | ~0.6 lbs/week |
| ≥30.0 | Obesity | 11–20 lbs | 1–5 lbs | ~0.5 lbs/week | ~0.5 lbs/week |
- Most people gain 1 to 5 pounds in the first trimester as early changes begin.
- Steady gain in the second and third trimesters is typical, guided by your BMI category.
- Calorie needs shift with time. No extra calories are usually needed in the first trimester, about 340 extra per day in the second, and 450 extra per day in the third.
- Weight gain supports fetal growth and prepares your body for delivery and breastfeeding.
Common Causes of Weight Loss in Pregnant Women
Weight may drop in early pregnancy for simple reasons such as nausea or taste changes. Healthier food swaps can also lower calories without effort.
How does morning sickness affect pregnancy weight?
Morning sickness causes nausea and vomiting, especially in the first trimester. Many people gain only a few pounds during these weeks, and some lose weight if they struggle to eat or drink.
Severe vomiting can lead to dehydration and low calorie intake. Hyperemesis gravidarum is a serious form of morning sickness with frequent vomiting, dehydration, and fewer bathroom trips. It can cause malnutrition without quick treatment.
Typical morning sickness improves later, and most people regain lost pounds as appetite returns. If eating and drinking stay hard, contact your provider for support.
How does pregnancy change metabolism?
Nausea and food aversions can change how and what you eat in early pregnancy. Soon after, your resting metabolism often increases, so you burn more calories even at rest.
Hormone shifts also affect fluid balance, which can cause quick scale swings that are not fat changes. These shifts help deliver extra nutrients to your growing baby.
Your appetite may vary by trimester as your body asks for more protein, iron, and other nutrients. These changes are normal and help meet rising needs for growth.
What diet changes lead to weight loss during pregnancy?
Small shifts can lower calorie intake fast. Swapping processed snacks for fruits, vegetables, and whole grains usually cuts calories and adds fiber and vitamins.
Limiting soda and sweets reduces added sugars that raise total intake. Skipping meals can also cause weight loss, so spread small meals and snacks across the day.
Many people manage morning sickness with simple steps like avoiding strong smells and eating crackers after waking. That can help nausea, but calories may still fall if you do not plan balanced meals.
A friend of mine lost a few pounds in the first trimester after trading fast food for home-cooked meals and short walks. Her doctor tracked her progress using BMI-based charts to keep growth on target.
Safe Strategies for Weight Loss During Pregnancy
Your goal is to protect fetal growth while caring for your own health. A tailored plan from your care team helps you manage calories, nutrients, and activity safely.
Why should I consult healthcare professionals about weight loss?
Your doctor or midwife monitors weight trends and screens for conditions like preeclampsia and gestational diabetes. They may refer you to a registered dietitian for a meal plan that meets pregnancy needs.
Providers can order labs if you feel weak or dehydrated. Treatments might include vitamin B6 for nausea or IV fluids when needed.
If you have overweight or obesity, your team can set goals that support steady fetal growth with lower risk. Get approval before new workouts, especially if you were inactive before pregnancy.
I once needed help for tough morning sickness. My doctor adjusted my nutrition plan and offered safe activity steps based on current obstetrics research. That support made a quick difference and kept my energy up.
How to choose nutrient-rich foods while pregnant?
Food quality matters more than perfection. Build plates that deliver key nutrients without extra empty calories.
- Fill half your plate with colorful vegetables and fruits. These add folate, fiber, and vitamins, and they help digestion.
- Choose whole grains like brown rice, oats, quinoa, and whole wheat bread for steady energy.
- Pick lean proteins such as chicken, low mercury fish, tofu, beans, or eggs to support fetal growth.
- Include dairy or fortified alternatives for calcium and vitamin D to support bone health.
- Swap sugary drinks for water. Aim for at least 8 cups per day to stay hydrated.
- Trade processed snacks for fruit, nuts, or yogurt to limit empty calories.
- Use olive oil instead of butter, and reduce fried foods to manage saturated fat.
- Read nutrition labels. Look for higher fiber and less added sugar and sodium.
- Take a prenatal vitamin as your OBGYN recommends to cover any gaps.
These habits help you maintain a healthy weight through each trimester while fueling your child’s development.
How can I manage calorie intake safely during pregnancy?
You can match calories to your needs without extreme dieting. The steps below support stable energy and growth.
- Set goals with your OBGYN or midwife, especially if you have overweight or obesity. This lowers risks linked to cesarean delivery and other complications.
- Track meals with labels or a simple app to watch portions and added sugars.
- Increase calories in the second and third trimesters, usually about 300 to 450 extra per day based on your provider’s guidance.
- Eat smaller, regular meals instead of skipping. This helps blood sugar and reduces fatigue.
- Choose healthy fats such as olive oil, avocado, nuts, and seeds for steady energy.
- Limit sugary condiments and high-salt sauces that add calories without nutrients.
- Drink water throughout the day. Good hydration supports metabolism and reduces headaches.
- Listen to hunger and fullness cues. Avoid undereating due to stress or busy days.
Following these basics helps you meet calorie and nutrient needs for both you and your baby.
How much water should I drink to stay hydrated?
Most experts recommend 8 to 12 cups of water daily, or about 64 to 96 ounces. You may need more in hot weather or if nausea and vomiting make you lose fluids.
Water supports metabolism, digestion, and healthy blood flow. It can also lower your chance of urinary tract infections, which are more common in pregnancy.
Keep a refillable bottle with you to track intake. If urine looks dark or you feel thirsty often, increase fluids. Small sips throughout the day usually work best.
Strong hydration also makes it easier to enjoy nutrient-dense foods and reach your pregnancy weight gain goals.
Effective Exercises for Managing Pregnancy Weight
Moving your body can lift mood, ease pain, and help manage weight. Think of exercise as a tool that supports you and your baby.
What are the benefits of walking during pregnancy?
Walking is gentle on joints and easy to start. It helps control weight gain, supports heart health, and may reduce back pain and swelling.
Short walks count. Try 10-minute sessions, two or three times a day. Many people find this pattern easier as pregnancy progresses.
Regular walks improve circulation, which supports your baby’s well-being. Studies link prenatal activity to better overall fitness through pregnancy and into the postpartum period.
How does swimming help pregnancy fitness?
Swimming supports your body weight, so it reduces stress on hips and knees. Water also helps prevent overheating, which makes longer sessions more comfortable.
Many people notice less ankle and foot swelling after pool time. Gentle laps and water walking can raise heart rate without joint strain.
Stretching in the water can increase flexibility safely as your belly grows. Lower stress is a common bonus, and that can help sleep and mood.
Healthcare professionals often rate swimming as one of the most comfortable options across all trimesters, especially when walking feels hard late in pregnancy.
What are the basics of prenatal yoga and Pilates?
Prenatal yoga builds flexibility and eases common aches. Breathing practice can help you manage labor and improve sleep. A 2012 study found prenatal yoga lowered stress and improved rest quality.
Prenatal Pilates strengthens your core and pelvic floor. These muscles support posture changes and prepare your body for delivery.
Choose classes built for pregnancy or ask qualified instructors for modifications. Avoid poses that compress the belly or strain your back and neck.
When I tried prenatal Pilates at six months, simple bridges and clamshells eased my lower back tension without discomfort. Many parents report fewer aches and better mood with regular practice.^1 This aligns with guidance from The American College of Obstetricians and Gynecologists.
Safe movement helps prevent excessive weight loss while improving healthy weight management through each stage.
…
1: ACOG Committee Opinion No 650: Physical Activity And Exercise During Pregnancy And The Postpartum Period (December 2015)
Which light strength training exercises are safe?
Light resistance work maintains muscle, which supports joints and prepares you for labor. Try band rows, wall push-ups, and light dumbbell curls.
Breathe normally during each move. Stop if you feel pain, dizziness, or shortness of breath. Avoid lying flat on your back after 12 weeks to protect blood flow.
Check with your provider before starting. A certified prenatal trainer can help you adjust exercises for each trimester and teach proper form.
My doctor suggested two gentle strength sessions per week. That plan eased back pain, improved posture, and supported steady, healthy gain without strain.
Nutritional Tips for a Healthy Pregnancy
A balanced plate helps you feel better and fuels your baby’s growth. Smart choices are practical, tasty, and easy to repeat.
Which fruits, vegetables, and grains are essential?
Fruits rich in vitamin C, such as oranges and strawberries, help your body absorb iron. Apples and blueberries add fiber and antioxidants for digestion.
Bananas supply potassium for muscle function. Dark leafy greens like spinach and kale provide folate, which helps form the baby’s brain and spine.
Colorful vegetables such as broccoli, sweet potatoes, carrots, and bell peppers add vitamins A and C. Whole grains like brown rice, oats, barley, quinoa, and whole wheat bread give steady energy and support blood sugar control.
During my last pregnancy, oatmeal with berries kept me full until lunch and was easy to prepare. Variety at each meal helps you cover your bases, a point reinforced by current CDC and ACOG guidance.
Why avoid processed and sugary foods when pregnant?
Chips, candy, and sugary drinks add calories without important nutrients. These choices can push weight gain too fast and raise the risk of gestational diabetes.
Cutting soda and sweets helps you manage weight and blood sugar. Focus on whole foods so you get vitamins, minerals, and fiber without extra additives.
Fewer processed foods supports steady energy and a healthier pregnancy.
How to select healthy proteins and fats?
Choose lean protein like chicken, turkey, eggs, beans, tofu, and low mercury fish. These foods provide amino acids, the building blocks for growth.
Cook animal proteins well to prevent foodborne illness. Aim for two to three servings per day, or follow your provider’s advice.
Pick healthy fats such as olive oil, avocado, nuts, seeds, and salmon for omega-3s. These fats support brain development and help you feel satisfied.
Limit saturated fats from fried and highly processed foods to protect heart health.
The next section covers prenatal vitamins and how they fill gaps in your diet.
Why are prenatal vitamins important?
A daily prenatal vitamin supplies nutrients your diet may miss. Folate helps prevent serious brain and spine defects. B vitamins support both your energy and fetal growth.
Many people also need extra iron during pregnancy. My doctor recommended a brand after labs showed low iron in my second trimester. My energy improved within weeks.
Take your prenatal vitamin as directed. This simple step backs up your food choices and supports healthy development.
Managing Weight Concerns During Pregnancy
Staying on top of weight changes protects both you and your baby. Simple tracking and quick action make a real difference.
When should I seek professional advice about weight?
Call your provider if you feel dizzy, weak, or cannot keep food and fluids down. Get medical guidance before trying to lose weight during pregnancy.
Ask for a referral to a registered dietitian for a safe eating plan. Reach out immediately if weight drops fast or you notice reduced fetal movement.
Roughly 18 percent of pregnant people report nausea severe enough to affect nutrition in the first trimester.^1 Early help prevents low birth weight and nutrient deficits.
…
^1 March of Dimes (2022): “Nausea and Vomiting During Pregnancy.
How to track weight with an OBGYN?
Use the same home scale and record weekly weights. Bring your log to prenatal visits so your OBGYN can compare results with CDC weight gain charts.
Your provider will review trends by trimester, health history, and BMI. If gains or losses fall outside targets, they may adjust nutrition, activity, or order lab tests.
Many people feel calmer when they see steady data. Regular tracking catches changes early and supports safer outcomes for you and your child.
How to manage gestational diabetes effectively?
Eat balanced meals with fiber, lean proteins, and healthy fats to steady blood sugar. Most doctors suggest smaller, more frequent meals and plenty of water.
Screening usually happens around weeks 24 to 28. If diagnosed, careful weight management and approved exercise, such as walking or swimming, can lower risks for both of you.
I met with a nutritionist who helped me plan simple recipes and grocery lists. Some people need medication, including insulin, if diet and activity are not enough. Your care team will guide each step.
Risks of Excessive Weight Loss in Pregnancy
Losing too much weight can affect your baby’s growth and health. Knowing warning signs helps you act quickly.
How does losing too much weight affect fetal growth?
Excessive weight loss is linked with low birth weight. If you do not get enough calories, your baby may not receive key nutrients needed for growth.
Late pregnancy weight drops might signal poor fetal growth or low amniotic fluid. Both issues can harm your baby and lead to long-term concerns.
Conditions like hyperemesis gravidarum can cause severe vomiting and major weight loss. Research shows babies in these cases face higher risks after birth.
Warning signs include unusual fatigue or less fetal movement. Contact your provider right away if these symptoms appear with weight loss.
What signs indicate problematic weight loss, like fatigue or low fetal movement?
Excessive weight loss can disrupt development. Common signals show up before problems escalate.
Severe tiredness, dizziness, or weakness that does not improve with rest should prompt a call. Ongoing nausea and vomiting that prevent eating may cause dehydration and electrolyte imbalance.
Watch for reduced urination, dry mouth, or dark urine. These can point to hyperemesis gravidarum. Less baby movement is also urgent. Call your provider if kicks or rolls drop compared with usual patterns.
My OB asked me to track daily movements and call for any change in the second trimester. Studies show reduced activity can signal restricted growth.^1 Get medical care quickly if you notice these signs.
…
^1 American College of Obstetricians and Gynecologists (2022).
Common Myths About Pregnancy Weight Loss
Misconceptions spread fast. Clearing them up helps you make calm, informed choices.
What are common misconceptions about pregnancy weight loss?
Myth: every pregnant person should gain the same amount. In reality, targets change with your pre-pregnancy BMI. Myth: exercise is unsafe. Evidence shows moderate activity, like walking or swimming, supports healthy outcomes for you and your baby.
Myth: processed foods are harmless. They often add sugar and unhealthy fats that increase complications. Myth: losing a few pounds during pregnancy is always fine. Intentional weight loss is usually discouraged unless your care team recommends it for medical reasons.
After delivery, many people lose 10 to 15 pounds right away from the baby, placenta, and extra fluid. That is different from dieting during pregnancy.
How to balance weight and health during pregnancy?
Focus on steady habits. Choose leafy greens, fruits, whole grains, lean proteins, and healthy fats at meals.
Most providers aim for healthy weight maintenance and appropriate gain, not active loss, unless there is a clear medical need. Track intake, but do not go below trimester targets.
Include gentle activity like walking or prenatal yoga if your provider approves. Drink 8 to 12 cups of water per day to support circulation and digestion.
Regular check-ins help tailor advice based on blood pressure, glucose, and your growth pattern. Many parents find a simple food log or app keeps things easy.
Balancing calories and nutrients helps you meet pregnancy weight gain goals while protecting your health through each trimester.
Frequently Asked Questions on Pregnancy Weight Loss
Here are clear answers to common questions. Use them to guide everyday choices.
Why do some women lose weight in the first trimester?
Morning sickness is the main reason. Nausea, vomiting, and low appetite can lower calories and cause early weight loss.
Many people gain 1 to 5 pounds in these weeks, but some lose weight. Diet upgrades and small activity changes may also contribute. Certain medical conditions can play a part too.
I lost a few pounds in week eight due to nausea, then regained as I managed fluids and snacks. Early loss is often temporary unless symptoms persist or worsen.
What is the ideal pregnancy weight gain?
Early weight loss can happen, but healthy gain becomes the goal as pregnancy advances. The CDC recommends total gain based on your starting BMI. Underweight, BMI less than 18.5, aim for 28 to 40 pounds.
Normal BMI, 18.5 to 24.9, target 25 to 35 pounds. Overweight, BMI 25 to 29.9, aim for 15 to 25 pounds. With obesity, BMI 30 or more, a total of 11 to 20 pounds is often appropriate.[^1] For a BMI above 40, some clinicians may advise minimal gain.
Most people gain 1 to 5 pounds during the first trimester, then add weight more steadily later.[^2] Your OBGYN will check progress during visits and adjust goals as needed.
…
[^1]: Centers for Disease Control and Prevention: “Weight Gain During Pregnancy,” cdc.gov.
[^2]: Institute of Medicine: “Weight Gain During Pregnancy: Reexamining the Guidelines.
Is it safe to exercise while pregnant?
In healthy pregnancies, exercise is safe and helpful. Many guidelines suggest 30 to 60 minutes of activity on most days of the week.
Good options include walking, swimming, prenatal yoga, light jogging, and gardening. Regular movement can improve mood, sleep, and strength while supporting healthy weight gain and lower diabetes risk.
Ask your provider for clearance and any limits. I walked most mornings in my second trimester, which eased back pain and kept my energy steady.
Conclusion
A healthy pregnancy rests on simple daily choices. Eat nutrient-dense foods, keep moving with approved activities, and track progress with your OBGYN. These steps support healthy pregnancy weight gain while protecting your baby’s growth.
Seek help for rapid weight loss during pregnancy, ongoing vomiting, or less fetal movement. Your care team is there to guide you.
Disclaimer: This article is for education only. It does not replace medical advice. Always follow recommendations from your healthcare professional.
FAQs
1. Is it safe to lose weight while pregnant?
Doctors usually do not recommend intentional weight loss during pregnancy unless advised for specific medical reasons. Most health experts suggest focusing on healthy eating and moderate activity instead of dieting. Research from the American College of Obstetricians and Gynecologists shows that proper nutrition supports both mother and baby.
2. What are effective strategies for managing weight gain in pregnancy?
Eating balanced meals, choosing nutrient-rich foods, and staying active with doctor-approved exercise help manage weight gain safely. For example, walking or swimming can support heart health without straining the body. A 2020 study found that women who followed a structured meal plan gained less excess weight than those who did not.
3. How much should I eat each day when pregnant?
Calorie needs increase slightly during pregnancy but vary by trimester and individual factors like starting body mass index (BMI). The Centers for Disease Control and Prevention recommends an extra 340 calories per day in the second trimester and about 450 more in the third trimester compared to pre-pregnancy intake.
4. Can personal experience guide safe pregnancy weight management?
Personal stories often highlight challenges such as cravings or fatigue but also show how planning meals ahead helps maintain steady energy levels. One expectant parent shared that tracking daily food choices made it easier to avoid high-sugar snacks while still enjoying occasional treats.
Summary: Safe pregnancy weight management relies on evidence-based guidance from healthcare providers, balanced nutrition, regular physical activity suited to your condition, understanding calorie needs by trimester, and learning from others’ experiences to make informed decisions throughout gestation.







