Dietitian Vs. Nutritionist: Choosing The Right Registered Dietitian Nutritionist
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
You might wonder who to trust for food and nutrition advice, a dietitian or a nutritionist. A registered dietitian nutritionist is a health professional with strict education, supervised training, and skill in medical nutrition therapy, which is nutrition care used to treat health conditions.
This guide breaks down education, credentials, regulation, services, job outlook, and where each one fits. You will see what sets them apart so you can choose the right support for your goals.
Key Takeaways
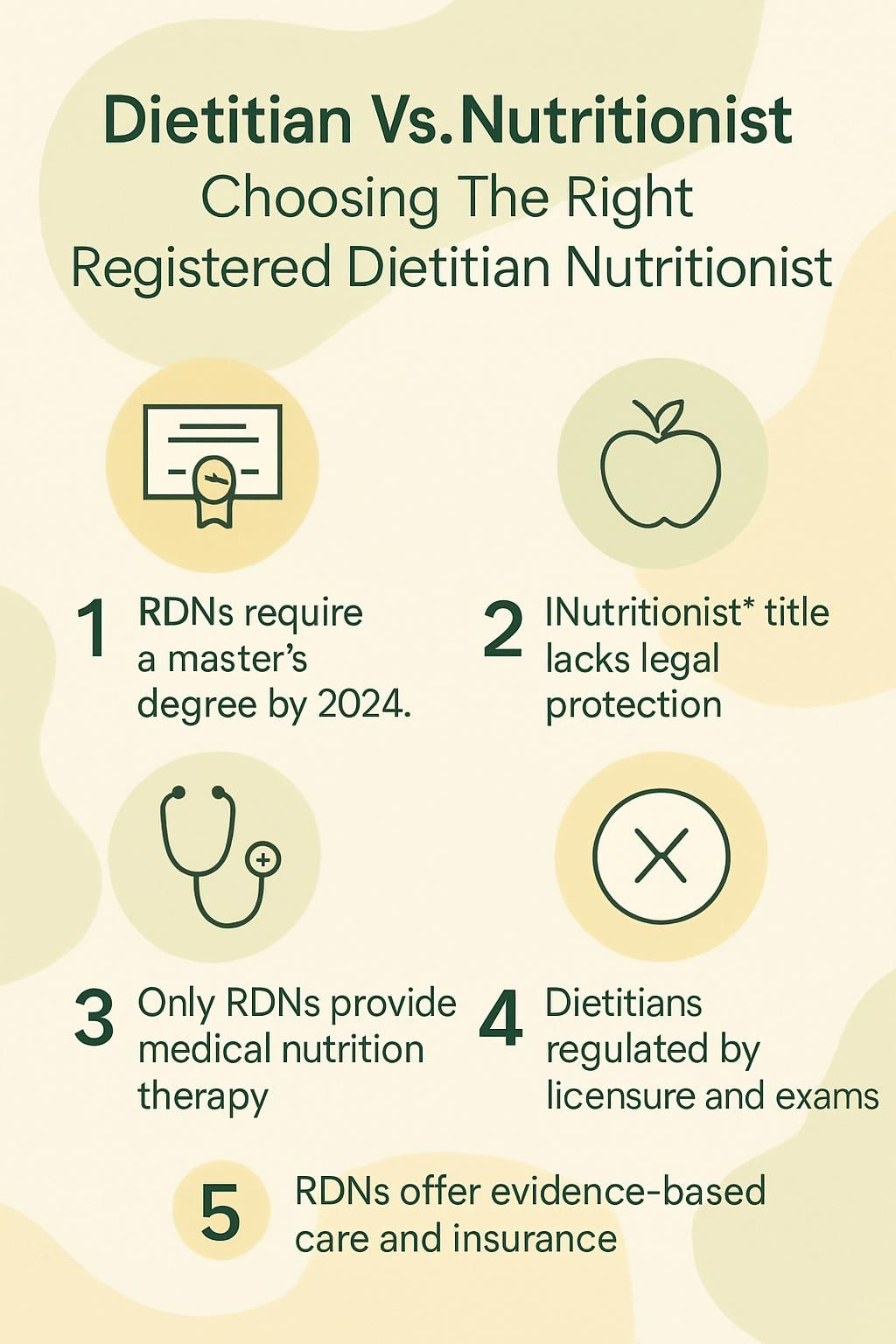
- Registered Dietitian Nutritionists, RDNs, must earn a master’s degree from an ACEND-accredited program and complete at least 1,000 supervised practice hours as of January 1, 2024.
- The title “nutritionist” is not protected in most states, so people with very different backgrounds may use it without a common standard.
- Only RDNs can provide medical nutrition therapy for conditions like diabetes, and they can bill insurance for clinical nutrition services in all 50 states.
- States regulate dietitians through licensure and a national exam by the Commission on Dietetic Registration, while rules for nutritionists vary widely or may not exist.
- Choose an RDN if you need evidence-based care, insurance coverage, or treatment for health conditions. General wellness advice from unregulated nutritionists may be fine for healthy individuals.
Understanding Dietitians

Registered dietitian nutritionists use nutrition science to guide healthy choices. Their education and training prepare them to support people with many health needs.
What is a registered dietitian (RD/RDN) and what do they do?
A registered dietitian is a health professional who specializes in food and nutrition to support well-being. You can find RDs in hospitals, clinics, long-term care, schools, private practice, and public health.
They use research from groups like the Academy of Nutrition and Dietetics to assess your needs, especially after surgery or during illness. Dietitians create personalized meal plans for conditions such as diabetes, kidney disease, and cancer.
Many also manage food service in clinics or cafeterias and supervise staff. During a hospital stay after my surgery, an RD built a clear plan that helped me regain strength faster than expected. These experts perform nutrition screenings, review lab reports, educate families, and deliver medical nutrition therapy as part of the care team.
The Bureau of Labor Statistics reports steady employment growth as more people seek help managing chronic disease through nutrition.
What education and training do dietitians need?
To become a dietitian, you must complete an ACEND-accredited degree in nutrition or dietetics. Courses cover biology, anatomy, physiology, chemistry, food science, human nutrition, and management.
Starting January 1, 2024, eligibility for the RD or RDN exam requires a master’s degree plus at least 1,000 hours of supervised practice through an accredited internship or coordinated program. Training occurs in hospitals, community clinics, schools, and sometimes corporate wellness programs.
After finishing coursework and supervised practice, you must pass the national exam administered by the Commission on Dietetic Registration. Continuing education is required to maintain RD credentials so dietitians stay current in clinical care and public health.
Many dietitians later specialize by earning certifications in areas such as sports nutrition or oncology after meeting additional requirements.
“Dietitians must meet rigorous academic standards before they ever counsel clients about food.”
How do dietitians get licensed and certified?
The path to becoming an RD or RDN includes completing an accredited degree and a supervised dietetic internship. After graduation, you must pass the national CDR exam to earn RD or RDN credentials. A master’s degree is required for new candidates beginning in 2024.
Many states require licensure, which allows you to use “LD,” Licensed Dietitian, after your name. Rules vary by state, so check local requirements before practicing.
To keep registration active, RDs complete continuing professional education every five years. Advanced roles include research and specialty practice in renal, pediatric, oncology, sports, diabetes education, and gerontology. These areas require added eligibility steps and separate exams.
Understanding Nutritionists
Nutritionists share guidance on healthy eating and lifestyle habits. Education, qualifications, and regulation for nutritionists vary widely across the United States.
What is a nutritionist and what is their general role?
A nutritionist plans and leads food or nutrition programs that promote health. You may meet nutritionists in hospitals, clinics, nursing homes, cafeterias, and government programs.
Their work centers on wellness education and basic dietary advice for issues like obesity, malnutrition, or food allergy. Many write educational materials, teach group classes, and help people make better food choices.
Nutritionists often monitor plans, document progress, and adjust advice as needed. Some run their own businesses and manage scheduling and records.
They commonly serve children, older adults, and people with chronic conditions by promoting better habits, balanced meals, and practical guidance for daily life.
How do nutritionists’ education and qualifications differ?
Training for nutritionists varies much more than for dietitians. Some states require a bachelor’s degree, while others accept short certificate programs.
The title “nutritionist” is often unregulated, so it does not always mean formal education in nutrition or dietetics. Some nutritionists hold a graduate degree, but it is not required in many places.
The Certified Nutrition Specialist, CNS, credential requires at least a master’s or doctorate in nutrition or a related health field, plus supervised experience and a national exam. Fewer employers require CNS compared with RDN. Acceptance depends on the job and the state.
States recognize these credentials differently. Some accept the CNS, while others do not. Many organizations also ask for continuing education to maintain certification.
Because requirements vary, check what services a nutritionist can legally provide in your state, especially for complex needs such as food allergies, kidney failure diets, feeding tube use, or cancer care.
What are the challenges in nutritionist regulation and certification?
In many states, the title “nutritionist” is not protected. Anyone may call themselves a nutritionist, even without formal training.
State rules vary widely. Some require registration or basic certification, and others do not regulate the title at all.
This lack of a standard leads to big differences in skill and training. The CNS is accepted in several states, but recognition is inconsistent.
Clients often struggle to verify qualifications. Fewer clear rules govern practice compared with dietitians who meet ACEND standards and pass the national CDR exam. Many employers prefer RDs or RDNs because of their rigorous internship and education.
These differences shape education, scope of practice, and legal limits for both roles.
Key Differences Between Dietitians and Nutritionists
Dietitians follow stricter education, internship, and certification requirements than nutritionists. Understanding these gaps can help you choose the right level of care.
How do their education and academic requirements compare?
Education and training for registered dietitians and nutritionists differ in structure and depth. This summary shows key contrasts in degree level, accreditation, and supervised practice.
| Criteria | Registered Dietitian (RD / RDN) | Nutritionist |
|---|---|---|
| Degree Level | Bachelor’s degree required until 2023 Master’s degree required from 2024, ACEND-accredited program | Varies by state Can range from certificate to bachelor’s or graduate degree |
| Required Coursework | Science prerequisites Anatomy, biology, physiology, chemistry | May include nutrition courses Science training not always required |
| Accreditation | ACEND accreditation mandatory | No national accreditation standard State-by-state regulation |
| Supervised Practice / Internship | Minimum 1,000 hours Supervised practice or coordinated program required | Not consistently required Varies widely by program |
| Certification Exam | Must pass national registration exam | Standardized exam not required Some optional certifications available |
| Licensure | Must meet state licensure requirements, where applicable | Varies by state Some states have no licensure for nutritionists |
During my supervised internship in dietetics, I spent hundreds of hours in clinical care. I learned science-based nutrition and managed complex cases under direct supervision. Nutritionist training may not require that hands-on experience and may focus more on general wellness than medical nutrition therapy.
The next section explains how credentials and certifications shape what each professional can do.
What are the differences in professional credentials and certifications?
Dietitians and nutritionists may look similar, but their credentials and certifications differ in important ways.
| Criteria | Registered Dietitian (RD/RDN) | Nutritionist |
|---|---|---|
| National Registration | Required. Must pass the Commission on Dietetic Registration, CDR, national exam. | Not required. Varies by state and certifying body. |
| Licensure | Required in most states. Must meet state-specific requirements. | May be optional or unavailable. State regulation inconsistent. |
| Minimum Education | Bachelor’s degree in an accredited dietetics program, plus supervised practice of at least 1,000 hours. From 2024, a master’s degree is required to sit for the exam. | No universal minimum. Some hold degrees, while others may have certificates or no formal education in nutrition. |
| Credentialing Organization | Commission on Dietetic Registration, CDR. | May hold Certified Nutrition Specialist, CNS, from the Board for Certification of Nutrition Specialists. Recognition varies. |
| Protected Title | “Registered Dietitian” and “Registered Dietitian Nutritionist” are protected titles. Only those who meet requirements may use them. | “Nutritionist” is not protected in most states. Anyone may use it in some regions. |
| Specialty Certifications | CSG, gerontological; CSSD, sports; CSP, pediatric; CSR, renal; CSO, oncology. | Limited recognition. Some may hold CNS or other specialty certificates. |
| Employer Preference | Hospitals, clinics, and many employers prefer or require RD/RDN credentials. | Fewer employers require a nutritionist credential. Recognition depends on role. |
| Scope of Practice | Can provide medical nutrition therapy, build care plans for specific diseases, and work in clinical settings. | Typically offers general nutrition advice. Cannot provide medical nutrition therapy unless allowed by state law. |
How do their scopes of practice and legal boundaries vary?
Scope and legal boundaries affect the type of care you can receive from each professional. Here is a summary of key differences shaped by law, education, and setting.
| Aspect | Registered Dietitian Nutritionist (RDN) | Nutritionist |
|---|---|---|
| Legal Authority | State licensure allows RDNs to provide medical nutrition therapy for disease management. RDNs are recognized in all 50 states. | Legal authority varies by state. Many states restrict medical nutrition therapy to RDNs. Some allow Certified Nutrition Specialists to offer expanded services. |
| Scope of Practice | Can assess, diagnose, and treat nutrition-related conditions. Authorized to develop clinical nutrition care plans. Supervise food service in regulated facilities. | Often limited to non-clinical advice, wellness coaching, and general healthy eating guidance. May not treat medical conditions unless state law permits. |
| Settings | Hospitals, outpatient clinics, skilled nursing, research, public health. Can bill insurance for medical nutrition therapy. | Gyms, wellness centers, corporate offices, private consulting. Insurance reimbursement is uncommon. |
| Certification | Must pass a national exam, complete supervised practice, and meet continuing education requirements. | Education and certification vary widely. “Nutritionist” is not a protected title in many states. |
| Professional Limitations | Can deliver individual, group, and community programs. Authorized to manage chronic conditions like diabetes and kidney disease. | Cannot provide disease-specific therapy in most states. Often focused on prevention and wellness. |
| Regulation | Regulated in all states. Violating scope can result in fines or loss of license. | Regulation is inconsistent. Some states have no rules. Others require CNS or similar for clinical practice. |
| Personal Experience | During recovery from a GI disorder, my RDN coordinated with my physician to adjust my meal plan. Insurance covered the visits. | I worked with a nutritionist for fitness goals and meal prep ideas. It was helpful, but I needed an RDN for medical advice. |
Roles and Responsibilities of Dietitians
Dietitians work in clinical care, communities, and management to support both patient and public health. They complete a degree and supervised internship before providing specialized nutrition care.
How do dietitians provide medical nutrition therapy (MNT)?
To deliver medical nutrition therapy, an RD or RDN first reviews your health, labs, and diet history. They use your diagnosis and test results to design a plan that fits your condition.
For diabetes or kidney disease, meal plans change based on your labs and symptoms. In hospitals and clinics, dietitians track weight, lab values, and tolerance to foods over time.
Early on, visits may be weekly as they monitor progress. Many insurance plans cover MNT when provided by licensed RDs or RDNs.
During my hospital recovery, a clinical dietitian reviewed my bloodwork with me and explained each food choice. That clear plan made new restrictions less stressful.
How do dietitians create personalized meal plans for health conditions?
Dietitians start with your health metrics, lab results, and a detailed diet assessment. Their advanced education and clinical training help them shape safe plans for medical needs.
For chronic kidney disease, an RDN may limit sodium, phosphorus, and protein while still providing enough calories. For eating disorders or malnutrition, they focus on nutritional rehabilitation and safe food reintroduction.
They consider your culture, preferences, allergies, and budget. Tools like food diaries or nutrient analysis help fine-tune the plan.
When I managed anemia, my dietitian used my labs to adjust iron-rich foods and vitamin C sources. Dietitians also teach families how to support the plan at home and update it as your health changes.
What is the dietitian’s role in healthcare teams and clinical settings?
You will often see registered dietitians in hospitals and nursing homes, which employ a large share of the field. They assess nutrition needs during illness and recovery.
Dietitians meet with doctors, nurses, and therapists to shape MNT plans. This includes advanced care like tube feeding or parenteral nutrition in intensive care.
Many supervise food service, document plans, and track progress. They also teach patients and caregivers for safe nutrition at home after discharge. Some help set hospital policies and manage special menus.
How do dietitians manage community health and wellness programs?
Community dietitians partner with public health clinics, health plans, and local agencies. They lead education in schools, workplaces, and government settings.
Using data, they design programs for groups such as teens or older adults. Campaigns may address obesity, food insecurity, or nutrition literacy.
During a school program I joined, dietitians created handouts, planned balanced menus, and tracked results. Management dietitians then used surveys and health statistics to refine the approach.
These efforts help communities gain access to science-based nutrition information and healthier foods.
Roles and Responsibilities of Nutritionists
Nutritionists often provide practical guidance in wellness and workplace settings. Their tips can help you build healthy routines that fit your life.
What general dietary advice do nutritionists offer?
Nutritionists teach basic healthy eating and simple planning skills. They help you read labels, shop smarter, and prepare meals that match your taste and budget.
Using evidence-based guidance, they create general plans for weight management and wellness. Common advice includes eating more fruits, vegetables, and whole grains.
They share behavior change strategies, like planning snacks or limiting added sugars. Some support sports goals, stress eating, or weekly meal prep.
This guidance is non-medical. It does not replace medical nutrition therapy used for specific diseases.
How do nutritionists educate clients on healthy eating habits?
Nutritionists use classes, workshops, and simple materials to build skills such as portion control, label reading, and smart shopping.
Group sessions may cover ingredient lists and better snack choices. In private visits, they set specific goals, like adding fiber or eating breakfast regularly.
They often provide handouts or online tools to support meal planning. Many use behavior counseling methods to help you handle cravings and busy schedules.
Progress is tracked with clear targets each week so you can see results.
Where do nutritionists typically work in wellness, fitness, or corporate settings?
Nutritionists work in wellness centers, gyms, and fitness studios. Many join corporate wellness programs to boost employee health.
Large employers hire nutritionists to run challenges, teach seminars, and create educational campaigns. Their training helps them build plans for active professionals.
Others choose self-employment, offering private consults or working with food brands and wellness startups. Some contribute to marketing or communications for health-focused companies.
Many also support athletes outside clinical settings with real-world fueling tips and simple recovery strategies.
What non-clinical nutritional guidance do nutritionists provide?
Nutritionists help healthy individuals with weight loss, sports nutrition, and plant-based eating patterns. They also guide meal prep and pantry organization.
Advice often includes hydration goals, safe supplement use, and balancing protein, carbs, and fats. Many explain food marketing tactics and the risks of fad diets.
When I worked with a nutritionist, I learned mindful eating and easy prep routines that fit a busy week. Insurance usually does not cover non-clinical services.
How to Choose the Right Professional for Your Needs
Start with your goals, then match the level of training you need. A clear plan makes it easier to pick the right expert the first time.
How do you assess your health goals and nutrition needs?
Begin by listing your top reasons for seeking help. You might need support for a condition like diabetes or kidney disease, weight goals, athletic performance, or general wellness.
Write down symptoms and concerns. If possible, review your medical history and recent labs with your physician. Note any issues that may require medical nutrition therapy.
Decide whether you need an RDN with clinical training or if general wellness guidance is enough. Insurance often covers dietitian services, especially for chronic conditions, and may require a referral.
These steps will guide you toward the right professional and ensure effective support.
When should you choose a dietitian instead of a nutritionist?
Choose a registered dietitian when your needs are medical or complex. Disease management, medical nutrition therapy, and post-surgery care call for an RDN.
Conditions such as diabetes, kidney disease, and cancer benefit from clinical expertise. Dietitians use advanced education and supervised training to build safe, research-based plans.
Hospitals and insurers usually require a licensed dietitian for pediatric, oncology, and geriatric care. Dietitians can interpret labs and coordinate care with your medical team.
If you want plans grounded in clinical research and need insurance coverage, an RDN is the best fit.
How can you verify credentials and experience before hiring?
Ask if the professional holds RD or RDN credentials if you need a dietitian. This confirms a degree in dietetics, supervised practice, and a national exam.
Look for specialty certifications like CSG, CSSD, CSP, CSR, or CSO to match your needs. Check for state licensure, such as LD, where required.
Use the Academy of Nutrition and Dietetics directory to find accredited dietitians. For nutritionists, request proof of degree, certification, and supervised experience.
When possible, ask for CNS credentials. Review continuing education, testimonials, and references. These steps help you judge quality before you decide.
Benefits of Working with a Registered Dietitian Nutritionist (RDN)
An RDN blends science with practical coaching, which helps you make steady changes that last.
Why is RDN advice considered evidence-based and science-backed?
RDNs rely on current research to guide every recommendation. Each one completes an accredited degree, at least 1,000 supervised hours, and the CDR national exam.
Ongoing education keeps them current with new guidelines. Their advice follows national standards designed to prevent disease and improve health with medical nutrition therapy.
When I worked with an RDN for diabetes management, the plan reflected peer-reviewed studies, not trends. That approach made choices clearer and outcomes better.
What nutritional assessments and monitoring do RDNs provide?
RDNs use screenings, lab reviews, and diet analyses to assess needs. You may track food intake or nutrients as part of care.
They create individualized plans and monitor progress with weight, symptoms, and lab results. Plans change as your health improves or new concerns arise.
My dietitian asked me to log meals in a phone app so she could track sodium for blood pressure. RDNs also coordinate updates with your other providers for integrated care.
How do RDNs manage chronic conditions and diseases?
RDNs use medical nutrition therapy to manage diabetes, kidney disease, heart disease, cancer, and eating disorders. They review labs and medical data to guide meal plans.
Care settings include hospitals, clinics, and outpatient centers. Some RDNs become Certified Diabetes Care and Education Specialists for focused blood sugar support.
When I was diagnosed with type 2 diabetes, my RDN adjusted food choices based on lab trends and taught my family how to help. Insurance often covers these visits.
What specialized nutrition programs and therapies can RDNs offer?
RDNs offer sports nutrition, pediatric care, renal support, oncology nutrition, and weight management. Many hold specialty credentials such as CSG, CSSD, CSP, CSR, or CSO.
They also support digestive health with plans such as gluten-free or low-FODMAP diets. Some guide intensive nutrition support for critical care or eating disorder recovery.
Community programs led by RDNs improve access to healthy foods for at-risk groups. Many also teach group classes and contribute to research so care stays current.
Common Misconceptions About Dietitians and Nutritionists
Myths blur the difference between these roles. Clarity helps you get the right level of care.
What myths exist about dietitians’ and nutritionists’ roles and expertise?
Many people think dietitians and nutritionists are the same. Only RDNs complete standardized training and supervised practice.
Another myth claims all nutritionists can provide medical nutrition therapy. In most states, only RDs or RDNs can legally deliver MNT.
Some believe dietitians only work on weight loss or only in hospitals. RDNs practice in schools, government, private clinics, sports, pediatrics, and oncology.
People also assume dietitians give generic advice. In reality, RDNs design personalized plans based on clinical evidence, and many insurance plans cover these visits.
Doctors are not the only experts on nutrition. RDNs are trained to manage nutrition for chronic disease, conduct assessments, and run wellness programs.
Are dietitian and nutritionist services expensive or hard to access?
Dietitians work in many locations, including hospitals, clinics, schools, and community programs, which improves access. Telehealth expands availability in many areas.
Costs vary by location and service type. State licensing rules can affect availability. Many employers and insurers cover registered dietitian services for medical nutrition therapy, and some offer sliding scale fees.
Scholarships and grants help train more dietitians, which supports local access. Demand has grown with an aging population; hospitals and outpatient centers are hiring. Many RDNs offer budget-friendly plans that match your needs.
Specialized Areas of Dietitian Practice
Many dietitians pursue advanced training in sports, pediatric, renal, and oncology nutrition. Specialty skills help them solve focused problems with precision.
What is sports nutrition and how do dietitians contribute?
Sports nutrition supports athletes and active people. An RDN reviews your fitness goals, training schedule, and energy needs.
You get meal plans for performance and faster recovery. During heavy training weeks, you might need more carbohydrates and special hydration strategies for hot weather.
RDNs use current research to shape simple, effective tactics. Their rigorous education and certification set them apart from many non-clinical providers.
How do dietitians support pediatric nutrition?
RDNs assess growth and development and build plans for children’s unique needs. They manage conditions like obesity, food allergy, and diabetes.
Many hold a master’s degree or a pediatric specialty credential, CSP. Parents and caregivers get coaching on healthy habits and practical meal ideas.
In hospitals, dietitians work with doctors and nurses to support complex cases. Look for RD or RDN credentials to confirm training and licensure.
What role do dietitians play in renal nutrition?
Dietitians guide people with chronic kidney disease through every stage of care. Plans focus on controlling sodium, potassium, and protein while meeting calorie needs.
They assess your current diet, coordinate with your care team, and adjust foods as labs change. Education materials help you understand what supports better outcomes.
In my family, an RDN’s plan helped my uncle manage kidney disease more confidently. Demand for renal dietitians continues to rise as the population ages.
How do dietitians assist in oncology nutrition?
RDNs support people during cancer treatment. They address side effects from chemotherapy and radiation with detailed assessments and personalized plans.
Their goal is to maintain strength, stabilize weight, and support recovery. Dietitians monitor your response and adjust plans as needs change.
They also teach safe food practices to reduce infection risk. Cancer teams rely on RDNs for evidence-based strategies to manage poor appetite and nutrient gaps. Employment for dietitians is projected to grow due to rising need for specialized care.
Questions to Ask Before Hiring a Dietitian or Nutritionist
Prepared questions help you find the right match. A short conversation can reveal training, fit, and approach.
What certifications and specialties should you inquire about?
Ask about RD or RDN credentials. These confirm an accredited degree, at least 1,000 supervised hours, and a national exam by the Commission on Dietetic Registration.
If you need advanced support, ask about specialties such as CSG, CSSD, CSP, CSR, or CSO. Confirm experience with your condition.
Some professionals hold the CNS title, which requires an advanced degree in nutrition. Recognition varies by state. When I planned diabetes care, I asked my dietitian about her training, and her board certification helped me feel confident.
How can you find out if they have experience with your health needs?
Ask whether they have worked with clients who share your health concerns. Request details about relevant cases and outcomes.
Confirm RD or RDN status, and review degrees in dietetics. Use the Academy of Nutrition and Dietetics directory to verify credentials.
Check if they use counseling strategies that fit your style. Professionals in hospitals often manage complex issues, while private practices may focus on prevention and wellness.
What approaches do they use for meal planning and counseling?
Dietitians gather your medical history, labs, lifestyle, and preferences before designing a plan. For diabetes or kidney disease, meal plans target lab goals and symptom control.
They consider allergies, culture, and budget so the plan is realistic. This careful process comes from years of education and supervised practice.
Ongoing monitoring is part of care. When I worked to lower cholesterol, my dietitian adjusted my plan every few weeks to include new foods and fit my budget.
Many use visual aids, food diaries, and checklists to help you track progress. Evidence-based counseling supports long-term success.
The Future of Nutrition Professionals
Demand for qualified nutrition experts is rising. New tools and research are shaping how care is delivered.
Why is demand for RDNs growing in healthcare?
Nutrition plays a major role in preventing and managing chronic disease. Hospitals and clinics rely on RDNs to assess needs, build plans, and support recovery.
A master’s degree is now required for new RDNs, which reflects the high standards for the field. The Bureau of Labor Statistics projects 7 percent growth from 2023 to 2033.
Specializations such as sports and oncology nutrition are valued in clinical teams. RDNs raise care quality with targeted, evidence-based strategies.
How is technology and AI shaping nutrition counseling?
Technology helps RDNs assess patients efficiently and deliver care anywhere. Digital platforms analyze diet data, track progress, and suggest research-based plans that fit your life.
Telehealth offers access to experts when travel is hard. AI tools can scan large data sets quickly and help personalize nutrition advice.
When I used a tracking app, my dietitian could see my updates and send timely reminders for diabetes care. New software also helps RDNs stay current on research.
What new career opportunities exist in corporate and community nutrition?
More dietitians now consult with food companies to develop healthier products and lead consumer education. Many design public health campaigns that serve entire communities.
Community dietitians work in schools, senior centers, and nonprofits to improve wellness. Some manage programs for children or lead prevention workshops.
Self-employment is growing. You can work directly with clients, consult part-time, or partner with organizations. Specialty certifications help RDNs meet diverse needs on corporate and community teams.
Conclusion
Choosing between a dietitian and a nutritionist depends on your goals and health needs. If you need medical nutrition therapy or help with a condition, a registered dietitian nutritionist offers science-based care and recognized credentials.
Nutritionists can support general wellness and healthy habits, but training and legal authority vary. Always check credentials and state rules before you decide. This article is for education only, not medical advice. For diagnosis or treatment, work with a licensed healthcare professional.
FAQs
1. What is the difference between a registered dietitian nutritionist and a nutrition coach?
A registered dietitian nutritionist, or RDN, holds an accredited degree in food science, completes supervised practice hours, and passes a national exam. A nutrition coach may not have formal training or certification. The Commission on Dietetic Registration oversees RDN credentials.
2. Why should I choose a registered dietitian nutritionist for my health needs?
RDNs use evidence-based methods to guide clients toward better eating habits. They can help with medical conditions like diabetes or heart disease using proven strategies supported by research from organizations such as the Academy of Nutrition and Dietetics.
3. Are there any statistics showing how effective registered dietitian nutritionists are compared to other professionals?
Studies show that people working with RDNs often see greater improvements in blood sugar control and cholesterol levels than those who work only with general wellness coaches (Smith et al., 2020). In one study, 65 percent of participants improved their dietary patterns after regular sessions with an RDN.
4. Can you share an example where choosing an RDN made a difference?
After my father was diagnosed with high blood pressure, he met weekly with an RDN at our local clinic. She created meal plans based on his lab results and tracked his progress over three months; his blood pressure dropped into the healthy range without medication changes.
Summary: Registered dietitian nutritionists offer specialized knowledge backed by scientific research and clinical experience; they provide tailored advice for complex health issues while helping clients reach measurable goals through structured support.







