Effective Diabetic Diet Plan & Diabetes Meal Ideas
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
Managing blood sugar can feel heavy at times, especially if you are new to a diabetic diet plan. I have seen how a simple diabetes meal plan, with steady meal times, can calm daily swings in blood sugar. Small choices add up, and clear steps make life with diabetes easier to handle.
In this guide, I share what works for me. You will see how to plan meals and snacks, plus simple breakfast, lunch, and dinner ideas. The goal is better diabetes management with less stress and more confidence.
Use these steps to make healthy eating practical and repeatable.
Key Takeaways
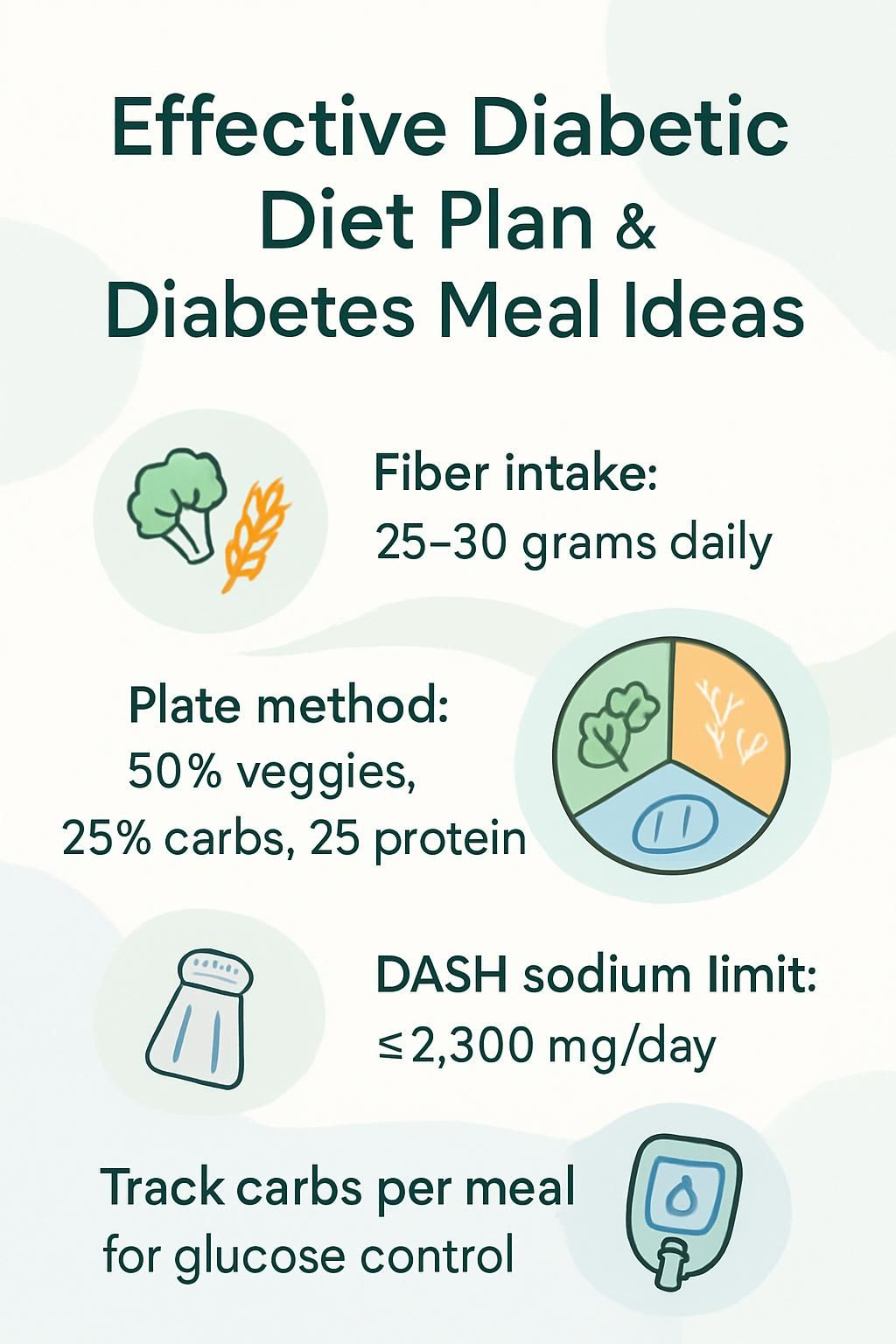
- A diabetic diet centers on balanced meals with nutrient-dense foods, smart portions, and 25 to 30 grams of fiber per day to steady blood sugar (American Diabetes Association, 2022).
- The Diabetes Plate Method guides each meal: 50 percent nonstarchy vegetables, 25 percent whole grains or other healthy carbs, and 25 percent lean protein.
- Carbohydrate counting, which means tracking total grams of carbs per meal, supports insulin matching and helps prevent spikes and drops in blood sugar.
- Hydration with water or zero-calorie drinks supports stable glucose. Sugary drinks raise risk for complications and can drive blood sugar higher.
- Mediterranean and DASH meal patterns favor whole foods, support heart health, and help control glucose. DASH also limits sodium to 2,300 mg per day.
Understanding a Diabetic Diet Plan

A clear plan is like a map for the day. I follow a diabetes diet plan to keep my blood sugar level in a safe range and to take the guesswork out of eating.
What is a diabetic diet?
A diabetic diet is a healthy eating plan that supports steady blood sugar level. It focuses on nutrient-rich foods, lower saturated fat, and smart calories. Health care providers and groups like the American Diabetes Association often recommend this plan for people with diabetes or prediabetes.
The core foods are fruits, vegetables, whole grains, lean protein, beans and peas, and low-fat dairy. I limit added sugars and avoid trans fat because those can raise cardiovascular risk.
I include moderate amounts of carbohydrates at set times. Regular meals help prevent sudden spikes or dips in glucose during the day.
Healthy fats from fish and nuts support heart health. That matters because heart disease risk is higher in people living with diabetes.
The strongest diabetic diets favor whole foods, balanced plates, and fewer high-calorie extras.
Why is meal planning important for managing diabetes?
Meal planning is a daily tool for managing type 2 diabetes and type 1 diabetes. A plan guides what I eat, how much I eat, and when I eat it. That rhythm helps keep my glucose steady across the day.
Regular, balanced meals reduce big swings in blood sugar. Planning also supports weight goals, which improves insulin sensitivity and can lower blood pressure and cholesterol.
Working with a registered dietitian helps me set portions that fit my activity and, if needed, my insulin. I focus on fiber and healthy fats from whole grains and omega-3 rich foods. That mix gives steady energy and lowers future risks.
Key Components of a Diabetic Diet
A healthy diet for diabetes blends quality carbs, lean protein, and healthy fats in portions that suit your routine. I build each meal with this balance in mind.
What are balanced macronutrients for diabetes?
Carbohydrates, protein, and fat each play a role. Carbs found in bread, cereal, rice, potatoes, and fruit raise blood sugar the fastest. Many educators teach a carb choice as about 12 to 15 grams of carbohydrate.
Protein from chicken, fish, eggs, tofu, or beans helps with fullness. Healthy fats from nuts, seeds, or avocado slow digestion of carbs, which smooths blood sugar after meals.
Pairing carbs with fiber-rich veggies or healthy fats steadies glucose. The plate method makes it simple: half nonstarchy vegetables, one quarter healthy starches, one quarter protein.
I track serving sizes so portions match my needs. That supports weight management and helps me keep meals balanced.
Think of carbs, protein, and fat as traffic signals for blood sugar: green for fiber-packed veggies, yellow for starchy carbs, red for added sugars.
How much should I eat? Understanding portion control
Portion control is often the difference-maker. I use hand-size visuals to estimate servings. Three ounces of meat or fish is about the size of my palm, and one ounce of cheese matches my thumb.
One cup or a medium fruit is close to my fist. One ounce of nuts fits in a cupped hand. These cues help me manage carbs without a scale at every meal.
Restaurant plates can be huge. Many entrées hold three or four servings. I often box half before I start eating.
At home, I measure snacks so portions stay realistic. Serving bowls stay off the table so second helpings are less tempting.
Research shows people eat more when portions are larger. These habits help me avoid overeating and keep blood sugar levels in range.
Why are dietary fiber and healthy fats important?
Fiber slows how fast food raises blood sugar. I reach for vegetables, whole fruit, nuts, beans, and whole grains. Getting 25 to 30 grams of fiber per day can help improve cholesterol and blood pressure, and it steadies glucose over time.
Healthy fats are also essential. Monounsaturated and polyunsaturated fats from avocados, nuts, canola oil, olive oil, and peanut oil can lower LDL, the so-called bad cholesterol.
Fatty fish like salmon and mackerel offer omega-3 fatty acids. Most experts suggest fish twice a week. I limit saturated fat from high-fat dairy and red meat and avoid trans fat to protect my heart.
The Diabetes Plate Method
The plate is a simple checkpoint I use at every meal. It keeps my eyes on balance, not perfection.
What does 50% non-starchy vegetables look like?
Half of a 9-inch plate is nonstarchy vegetables. I use salad greens, broccoli, carrots, tomatoes, spinach, or green beans. That space equals about 1.5 cups raw or 1 cup cooked.
The American Diabetes Association endorses this plate method to build balanced meals without constant measuring.
Filling half the plate with vegetables supports weight goals and helps control carbs. Then I add healthy carbohydrates to the next section.
Which healthy carbohydrates make up 25% of the plate?
Whole grains such as brown rice, quinoa, whole wheat bread, or oatmeal fit this quarter. Starchy vegetables like sweet potatoes and corn work here too. I might add half a baked sweet potato or roasted squash.
Fruit also fits. A small serving of berries or half an apple works well. Low-fat yogurt can count as a healthy carb.
I avoid white bread and other refined grains since they spike blood sugar faster and add less nutrition. I choose water or unsweetened tea with meals instead of sugary drinks.
Focusing on whole foods keeps my meal plan balanced and supports diabetes management.
What are good lean protein sources for diabetes?
One quarter of my plate is lean protein. I use chicken breast, eggs, tofu, tuna in water, beans, or lean pork. These choices have less saturated fat than fatty meats and support blood sugar control.
For example, a 3-ounce grilled chicken serving has about 26 grams of protein with only a few grams of fat. Plant proteins like tofu or beans fit well in a vegan meal plan.
My diabetes educator helped me see that lean proteins keep me full and aid steady glucose through the day. I skip bacon and hot dogs because they raise cholesterol and may increase heart risk.
Colorful vegetables pair well with these proteins. Next, learning what amounts to serve makes portion control easier.
Effective Meal Planning Tips for Diabetes
Planning ahead turns healthy eating into a routine, not a daily puzzle.
How can meal prepping and scheduling help manage diabetes?
Meal prep helps me keep balanced options ready. I plan meals with healthy carbohydrates, lean proteins, fiber, and healthy fats. Prepping stops emergency snacking on foods that can spike blood sugar.
Many educators suggest eating every 2 to 3 hours. This pattern prevents big spikes and dips in glucose.
Set meal times make portion control simpler. My care team helped me align my plan with patterns like the Mediterranean Diet or DASH Diet. A plan also keeps food costs in check.
What is carbohydrate counting and how do I do it?
Carb counting means tracking grams of carbohydrate in everything I eat or drink. Carbs raise blood sugar more than protein or fat. Counting helps me match carbs to insulin, if I use it, and avoid highs and lows.
For example, if breakfast has 30 grams of carbs, I use my prescribed insulin ratio to match it. My registered dietitian set a daily carb target that fits my diabetes diet plan.
I read labels for total carbs and measure portions. An app with a food database saves time because many items already list carb counts.
Counting gives better control after eating foods like milk, fruit, bread, pasta, or starchy vegetables. My care team helps me adjust for changes in activity.
Even small errors can change my readings. After months of practice, my numbers are steadier and I feel more confident with both vegan and low-fat choices.
How does glycemic index affect my meals?
The glycemic index, or GI, ranks carb foods by how fast they raise blood sugar. Whole fruit raises glucose more slowly than fruit juice. White bread and regular pasta spike faster than whole grains or beans.
Choosing lower GI foods reduces spikes after meals. I aim for beans, lentils, and nonstarchy vegetables more often.
My dietitian helps me pick carbs with a gentler effect. That gives steady energy without losing flavor or variety.
Lower GI choices can also support heart health, which matters for people with diabetes.
Breakfast Ideas for a Diabetic Diet
A steady breakfast sets the tone for the morning. I keep it simple and balanced.
How to make whole-grain toast with avocado and eggs?
I toast one slice of whole wheat bread for a slow-digesting carb. I mash ripe avocado on top for heart-friendly fat. Then I add one cooked egg for lean protein. This mix helps control blood sugar and keeps me full longer.
What are the benefits of Greek yogurt with nuts and berries?
Plain Greek yogurt gives me protein without added sugar. Nuts add healthy fats and fiber. Berries supply vitamins and slow-digesting carbs.
This combo keeps me satisfied and reduces sharp rises in blood sugar. It is a quick option on busy mornings.
Why choose oatmeal with chia seeds and almond butter?
Oatmeal is a whole grain that steadies blood sugar better than many breakfast bars. Chia seeds add fiber and healthy fats. Almond butter adds protein and more monounsaturated fat.
Foods high in fiber and healthy fat slow digestion of carbs. That can help prevent rapid glucose rises after eating [1].
I find oatmeal keeps me full for hours. It also makes portion control easier, which my health care provider supports.
[1] American Diabetes Association, 2022, Diabetes Superfoods.
Lunch Ideas for a Diabetic Diet
Midday meals keep my energy up and my glucose steady until dinner.
How to prepare a grilled chicken salad with leafy greens?
I fill a large bowl halfway with leafy greens like spinach or romaine. Nonstarchy vegetables should be half the plate.
Next, I add about 3 ounces of grilled chicken for lean protein. I drizzle a small amount of olive oil for healthy fat and toss in tomatoes or cucumber for extra fiber. If I need more energy, I add a small piece of fruit or a small whole grain roll.
What makes lentil soup with whole-grain crackers a good choice?
Lentil soup provides plant protein and fiber, which steady blood sugar. Lentils raise glucose more slowly than refined starches.
Whole grain crackers add a controlled portion of healthy carbs. I cap the number of crackers to keep carbs in range.
How to make a turkey and vegetable wrap with hummus?
I use a whole grain wrap for slower-digesting carbs. Sliced turkey breast adds lean protein that supports fullness.
I spread two tablespoons of hummus for healthy fats and fiber. Then I load spinach, shredded carrots, and tomato. These nonstarchy vegetables help me meet the plate method.
This wrap follows portion guidance and fits most diabetes meal plans. Your health care provider can help you adjust fillings to your needs.
Dinner Ideas for a Diabetic Diet
Evening meals are my chance to refuel without a glucose spike.
What is a healthy recipe for baked salmon with quinoa and broccoli?
I bake a 4-ounce salmon fillet at 400°F for about 15 minutes. I brush it with 1 teaspoon olive oil, lemon, and pepper to keep added fat low.
Half a cup of cooked quinoa fills the healthy carb quarter of the plate. I steam broccoli to cover half the plate with nonstarchy vegetables.
Fish like salmon provides omega-3s. This meal fits the plate method and gives steady energy without frying.
How to cook stir-fried tofu with mixed vegetables?
I press and cube firm tofu. I heat a tablespoon of canola or olive oil in a nonstick skillet. I brown the tofu for 3 to 4 minutes per side, then set it aside.
I add carrots, green beans, and broccoli to the skillet. A quick stir-fry keeps them crisp-tender. I season with low-sodium soy sauce instead of high-salt sauces.
I return the tofu and toss to coat. This dish balances plant protein, fiber, and healthy fat while limiting saturated fat.
Why choose grilled lean steak with roasted sweet potatoes?
Lean steak such as sirloin gives high-quality protein with less saturated fat. It helps support muscle and steady energy.
Roasted sweet potatoes add fiber and vitamins A and C. One quarter of the plate is enough. Sweet potatoes often have a lower glycemic load than many white potato types.
Studies show fiber-rich meals can reduce post-meal glucose spikes. I complete the plate with a generous serving of nonstarchy vegetables.
Diabetes-Friendly Snacks
Smart snacks protect me from dips between meals and curb cravings later.
What are the benefits of a handful of almonds or walnuts?
A small handful of almonds or walnuts, about 1 ounce, gives healthy fats, fiber, and protein. These nutrients help with fullness and heart health.
Nuts have a low glycemic index, so they do not raise blood sugar quickly. One serving fits into most diabetes meal plans.
How to enjoy sliced veggies with guacamole?
Carrot sticks and celery are great for dipping. I pair them with guacamole for fiber and heart-friendly fat from avocado.
Fiber and healthy fat together can support steady blood sugar. This snack keeps crunch without added sugars or refined starches.
Are low-sugar protein bars good snack options?
Low-sugar protein bars can work if I choose wisely. I look for less than 5 grams of added sugar and at least 10 grams of protein.
Protein with fiber helps control hunger for longer. I also drink water first to check if I was just thirsty.
On busy days, a good bar gives me energy without a spike. I read labels closely to avoid hidden sugars.
Special Considerations for Managing Diabetes Through Diet
Small daily habits often shape long-term results. These steps help me stay in range consistently.
How does hydration affect diabetes management?
Staying hydrated supports healthy glucose. I stick to water or zero-calorie drinks like unsweetened tea. Sugary drinks can raise blood sugar quickly.
Dehydration concentrates glucose in the blood, which can push readings higher. Drinking enough helps control appetite and supports weight goals.
Why monitor blood sugar before and after meals?
My numbers change before and after eating. Testing shows me how certain foods affect me. For example, white rice raised my glucose higher than brown rice.
Keeping values in range helps prevent nerve, kidney, and heart problems later. Tracking patterns lets me adjust sooner.
How to adjust meals based on physical activity?
I match my carbs to my activity plan. If I will walk briskly for 45 minutes or do a hard workout, I add a bit more carbohydrate before or after.
My registered dietitian helped me learn how to count those carbs. ADA guidance supports adjusting carbs with activity to manage glucose well.^1
If I use insulin, I work with my care team to adjust doses. On low-activity days, I reduce starchy foods and maintain vegetables and lean protein. This approach prevents spikes and crashes.
^1: American Diabetes Association, 2023, Standards of Care in Diabetes, Physical Activity.
Popular Diet Plans for Diabetes
Several eating patterns fit a diabetes meal plan. I choose the one I can follow most days.
What is the Mediterranean Diet and how does it help?
The Mediterranean Diet features vegetables, fruit, whole grains, beans, fish, and olive oil. It favors fiber and healthy fats and keeps added sugars low.
These foods support heart health and steady blood sugar. Focusing on plants makes portions satisfying without too many calories.
How does the DASH Diet support diabetes?
DASH highlights vegetables, fruit, and whole grains while holding sodium to 2,300 mg per day or less. It can lower blood pressure and reduce heart strain.
Eating fewer processed foods also cuts added sugar. Many people see better glucose and cholesterol with this pattern.
Are low-carb and ketogenic diets effective for diabetes?
Many studies link low-carb and ketogenic plans to lower blood sugar and improved A1C in the short term. Reducing bread, pasta, and other refined carbs often reduces spikes after meals.
Some people with type 2 diabetes lower insulin needs with medical guidance. Very low-carb plans do not suit everyone. Watch for fatigue or low fiber if you cut out whole grains.
Plant-forward versions can work too, using healthy fats, tofu, and careful portions of beans or lentils.
Common Mistakes to Avoid in a Diabetic Diet
Even good foods can work against you if portions or timing are off.
Why is overeating “diabetic-friendly” foods a problem?
Too much of any food can raise blood sugar. Restaurants often serve portions equal to several servings on one plate.
I measure snacks at home and avoid eating from the package. Portion size matters as much as food choice.
What happens if I skip meals or snacks?
Skipping meals can cause hypoglycemia, which means low blood sugar. I might feel shaky, dizzy, or confused.
Missing meals can also trigger a rebound high later. Regular meal timing keeps my energy steady and helps prevent swings.
How to identify hidden sugars and read food labels?
I check labels for added sugars like corn syrup, cane sugar, dextrose, or high-fructose corn syrup. Many yogurts and dressings include them even if the front claims low fat.
I compare Total Sugars and Added Sugars on the Nutrition Facts panel. The American Heart Association suggests women keep added sugar under 25 grams per day and men under 36 grams.
I look for less than 5 grams of sugar per serving and limit extras like sodium. Choosing items labeled no added sugar helps me stay in range.
Cooking at home gives more control. I still check sauces. Ketchup and pasta sauce can hide up to 8 grams of sugar in two tablespoons.
Benefits of Following a Diabetic Diet Plan
A steady plan improves energy and confidence. I see the difference in my daily numbers.
How does a diabetic diet improve blood sugar control?
Balanced meals with planned portions slow the release of glucose into the bloodstream. Studies show fewer spikes with consistent meals and correct portions.
Carb counting matters because carbs hit blood sugar the most. Fiber from beans, leafy greens, and whole grains slows digestion, which helps prevent rapid rises.
Regular meal times also help me predict how I will respond to different foods.
Can it reduce the risk of diabetes complications?
Keeping blood sugar controlled lowers the risk of nerve, kidney, and heart problems. Higher intakes of vegetables, fruit, and fiber link with lower cardiovascular risk.
Healthy dairy choices can support bone health. Portion control and steady habits reduce hyperglycemia and other long-term issues.
What overall health benefits can I expect?
Following a diabetes meal plan supports better insulin use and fewer highs and lows. Many people lose some weight, which improves A1C and blood pressure.
Right-sized portions lower daily calories without feeling deprived. Weight management helps reduce inflammation, protect the kidneys, and ease daily activity.
Staying hydrated lifts energy and supports digestion. This way of eating also lowers cholesterol and triglycerides over time.
Working With Professionals for a Customized Plan
Support makes the plan easier to follow, especially during changes in health or routine.
When should I consult a registered dietitian?
I reach out if I want a personal diabetes meal plan or if managing carbs feels hard. A dietitian teaches me portion skills, label reading, and carb counting I can use every day.
Your doctor can also refer you to diabetes education programs. Those sessions often include meal planning help.
How can diabetes educators assist me?
Diabetes educators tailor meal plans to my needs, taste, budget, and schedule. Many use Diabetes Self-Management Education and Support programs.
They teach carb counting, portion control, and how to spot added sugars on labels. I also learn how to monitor blood sugar before and after meals and adjust as needed.
These services appear in many clinics and hospitals. With their help, I prepare balanced meals and manage my condition with more confidence.
What are the best diabetes meal planning apps?
I like Diabetes Food Hub from the American Diabetes Association. It offers hundreds of recipes in English and Spanish, plus weekly plans and grocery lists.
Apps like MyFitnessPal and Carb Manager track carbs in detail. Many tools now add live cooking classes for diabetes-friendly meals. They save time and reduce guesswork.
FAQs about Diabetes Meal Planning
These answers cover common questions I hear most often about meal planning with diabetes.
What foods are best for people with diabetes?
Whole grains, beans, fruits, and vegetables build the base. I choose brown rice, quinoa, fresh fruit, low-fat dairy, and whole grain bread.
Fish like salmon or mackerel at least twice a week supports heart health. Lean proteins such as skinless poultry or tofu keep meals filling without much saturated fat.
How often should someone with diabetes eat?
I keep a steady rhythm, usually every 2 to 3 hours while awake. This pattern helps prevent large swings in glucose.
Waiting too long can lead to low energy and harder management. Consistent timing is a key part of any strong diabetes meal plan.
Can people with diabetes enjoy desserts safely?
I do enjoy desserts, and I plan for them with carb counting. I choose fresh berries or a small piece of dark chocolate without added sugar.
If I have cake, I adjust my insulin dose as my dietitian advised. Planning and small portions help keep glucose in range.
Conclusion
Following a thoughtful diabetes meal plan gives me structure and choice. Balanced plates, steady portions, and regular hydration support my blood sugar day after day.
Simple prep and clear routines make eating easier and more enjoyable. This information is educational and not a substitute for medical advice. Work with your health care provider for a plan that fits your needs.
FAQs
1. What foods should I include in an effective diabetic diet plan?
Choose whole grains, lean proteins such as poultry or fish, non-starchy vegetables like broccoli and spinach, and healthy fats from sources such as olive oil or nuts. These foods help control blood sugar levels while providing essential nutrients.
2. How often should people with diabetes eat meals each day?
Eating three balanced meals at regular times helps maintain steady blood glucose levels. Some individuals may benefit from small snacks between meals if recommended by a healthcare provider.
3. Are there specific meal ideas for someone managing diabetes?
Yes; try grilled chicken salad with leafy greens, brown rice with steamed vegetables and salmon, or scrambled eggs with tomatoes and whole grain toast. Each option offers fiber, protein, and controlled carbohydrates to support stable blood sugar.
4. Can following a diabetic diet plan improve long-term health outcomes?
Research shows that consistent adherence to a structured eating pattern can lower the risk of complications related to diabetes such as heart disease or kidney issues (American Diabetes Association). A patient once shared that after switching to planned meals rich in fiber and low in added sugars their energy improved within weeks.
Summary: An effective diabetic diet focuses on nutrient-rich foods eaten at regular intervals throughout the day; this approach supports better glucose management and reduces risks linked to diabetes over time.







