Essential Guide To A Diabetic Diet For Managing Diabetes
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
Eating healthy meals with diabetes can feel confusing at first. I used to wonder which foods would steady my blood sugar and which would send it soaring. The good news is that a clear meal plan built on simple steps can help keep glucose in range.
This essential guide shares practical tips, quick choices, and small habits that add up. I draw on evidence from the American Diabetes Association and the Centers for Disease Control and Prevention. My goal is to make healthy eating for diabetes easier to follow in daily life.
Use these ideas to pick better foods, build a realistic meal plan, and create routines that support long-term health. This article is educational and does not replace medical advice from your clinician.
Key Takeaways
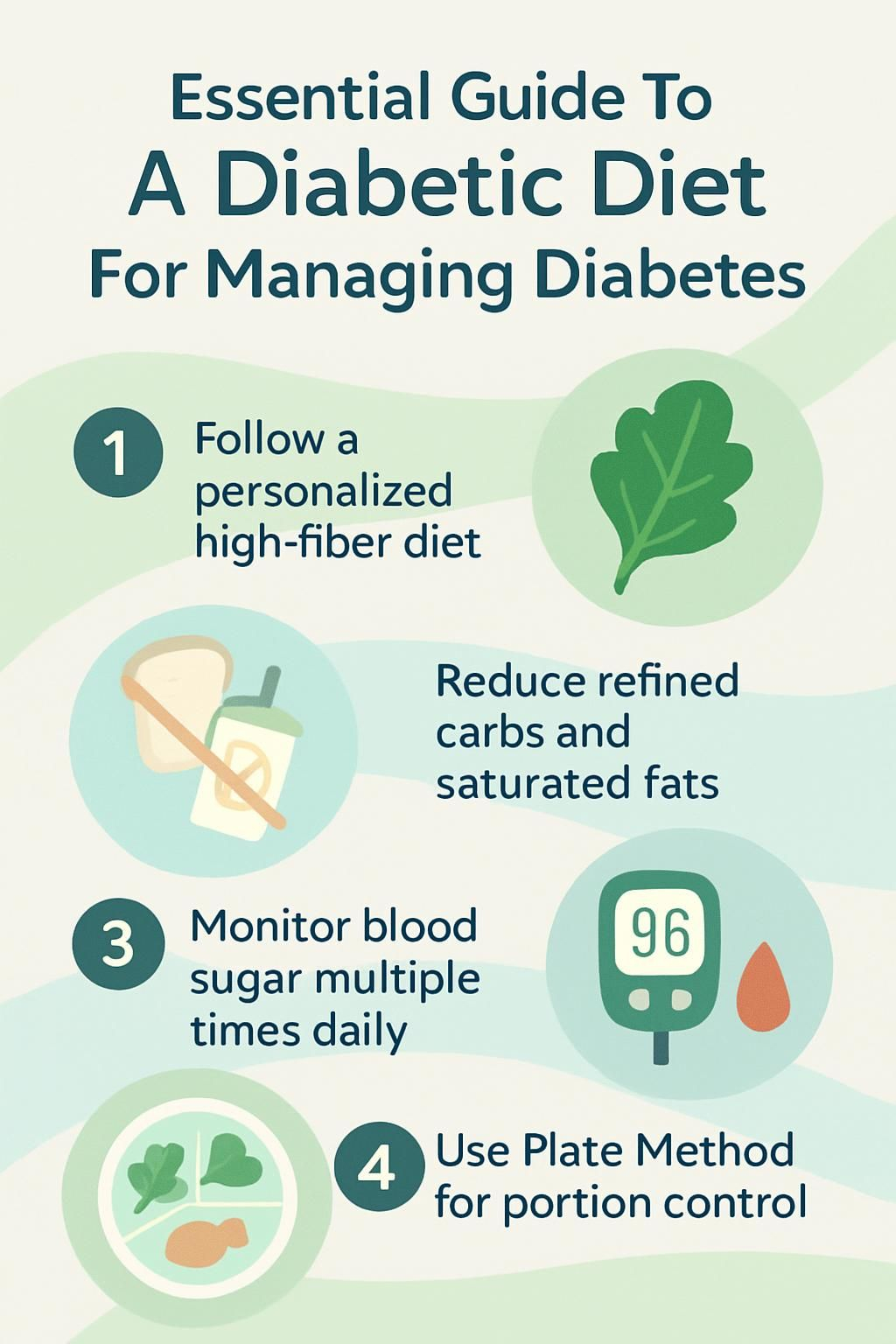
- A personalized diabetic diet with high-fiber foods, lean protein, whole grains, and limited added sugar helps keep blood glucose steady, according to guidance from the American Diabetes Association and CDC.
- Research shows that cutting refined carbohydrates and saturated fats while choosing nutrient-dense foods lowers the risk of heart disease and diabetes complications by about one third.
- Checking blood sugar several times per day with a meter reveals trends you can act on. Tools such as MyFoodAdvisor from the ADA can help you adjust meals based on readings.
- Consistent meal timing, portion control with the Plate Method, and two weekly servings of omega-3 fish support weight control and heart health.
- National Institute data from 2023 show that losing 5 to 10 percent of body weight can improve blood sugar and help prevent type 2 diabetes.
What is a diabetic diet and why is it important?

A diabetic diet is an eating plan that helps manage blood sugar levels with smart food choices. It supports daily diabetes care and lowers the chance of long-term problems linked to high glucose.
What does a diabetic diet mean?
A diabetic diet means I build a personal eating plan that keeps my blood sugar steady and supports overall health. The plan centers on nutrient-dense foods like non-starchy vegetables, whole grains such as brown rice, lean protein, and healthy fats.
I choose meals low in added sugar and rich in fiber to help my heart and blood vessels. The CDC suggests three balanced meals each day, with planned snacks if needed. There is no single plan for everyone. A registered dietitian helped me use the Plate Method and carb counting to fit my needs and tastes.
My goal is steady glucose through the day while enjoying a mix of foods from all food groups.
Why is managing blood sugar important for diabetes?
Food choices affect blood sugar directly. Balanced eating helps me avoid sharp spikes, called hyperglycemia, and dips, called hypoglycemia. High glucose over time can harm nerves, eyes, kidneys, and the heart.
The American Heart Association notes that poor glucose control raises the risk of cardiovascular disease. Regular meals with consistent amounts of carbohydrate support better insulin action and more even energy.
For people with prediabetes, nutrient-dense eating lowers the chance of developing type 2 diabetes¹. Weight loss helps too. Even a small loss improves glucose control, according to data from the National Institute of Diabetes².
Careful management protects long-term health and reduces complications related to diabetes.
¹ Source: Diabetes Prevention Program (DPP), NIH
² Source: National Institute of Diabetes and Digestive and Kidney Diseases
Key principles for a diabetic diet
Balanced meals act like a steady rhythm for your blood sugar. These principles make daily choices simpler and more consistent.
Why choose nutrient-dense foods?
Nutrient-dense foods give me vitamins, minerals, and fiber without too many calories or harmful fats. Fruits, vegetables, whole grains, beans, lean proteins like fish and chicken, and low-fat dairy help keep blood sugar steady while adding needed fiber.
Studies link diets rich in these foods with a lower risk of heart disease and better markers of glucose control. I reach for options like carrots, peas, beans, and omega-3 fish such as salmon or sardines. Choosing these foods supports a healthy weight and can also improve cholesterol.
How to reduce refined carbohydrates?
After focusing on nutrient-dense foods, I cut refined carbs to avoid sharp glucose spikes. These steps make a clear difference.
- I swap white rice for brown rice, quinoa, or other whole grains. Extra fiber slows how fast glucose enters my blood.
- I choose whole grain breads, tortillas, and pasta instead of white flour versions to lower the glycemic impact.
- I scan labels for added sugars and aim for less than 5 grams per serving. Sweets like candy, cookies, and cake are rare treats.
- I skip regular soda and sweet tea. Water, unsweetened coffee, or tea are my go-to drinks.
- I pick cereals labeled whole grain or high fiber and avoid low-fiber, sugary boxes.
- I use non-starchy vegetables instead of white potatoes or fries at most meals.
- I limit processed snacks such as chips and crackers that use refined flour and poor-quality oils.
- I build balanced plates with vegetables and whole grains using the Plate Method.
- I choose plain milk or yogurt to avoid added sugars in flavored versions.
- I track carbs at meals and aim for about one quarter of my plate as carbs, similar to MyPlate guidance.
Small changes each day reduce glucose spikes and support long-term diabetes care.
How to balance macronutrients effectively?
Macronutrients are carbohydrates, protein, and fat. I balance them to keep blood sugar and hunger steady.
- I choose quality carbs: whole grains, starchy vegetables, beans, fruit, and low-fat dairy. Fiber helps prevent fast rises in blood sugar.
- I include lean protein at every meal, such as skinless chicken, fish, eggs, tofu, or beans. Protein supports fullness and muscle.
- I add healthy fats from olive oil, canola oil, nuts, seeds, and avocados. Omega-3 fats from fish support heart health.
- I limit saturated and trans fat from processed meats and fried foods. Plant proteins and healthy oils are safer for my heart.
- I watch serving sizes. Using my hand or a measuring cup helps prevent overeating.
- I aim for half the plate as non-starchy vegetables, then one quarter lean protein and one quarter quality carbs.
- I adjust portions as my weight, medicine, or activity level changes.
Balancing these groups makes day-to-day glucose management easier.
Why monitor portion sizes?
Portion control helps keep my blood sugar steady. Large servings, even of whole grains or lean protein, can still raise glucose.
My dietitian taught me that one serving of starch, fruit, or milk has about 12 to 15 grams of carbs. Knowing this made carb counting and meal planning simpler and safer.
Accurate counts are vital if I use insulin. Reading labels and learning serving sizes protect my health while letting me enjoy a wide range of foods.
With portion control in place, it is easier to pick the best foods from each group every day.
Important food groups for managing diabetes
The right mix of food groups supports steady glucose and better energy. Here is how I build each plate.
How to include non-starchy vegetables?
Non-starchy vegetables give me fiber, vitamins, and minerals with very few carbs. They help keep my glucose level stable.
- I fill half my plate with options like broccoli, carrots, tomatoes, or cauliflower at most meals.
- I snack on cucumbers, bell peppers, or cherry tomatoes instead of sugary treats.
- I add leafy greens to sandwiches or wraps for extra crunch without raising blood sugar.
- I serve roasted Brussels sprouts or steamed green beans with a lean protein.
- I enjoy vegetable soups with tomatoes, spinach, and zucchini to boost fiber.
- I stir-fry mushrooms and snap peas in a small amount of olive oil.
- I pick fresh or frozen vegetables more often than canned to limit extra salt and sugar.
- I try swaps like cauliflower rice or zucchini noodles instead of refined pasta or white rice.
Which low-sugar fruits are best?
After loading my plate with greens, I reach for fruit that is sweet yet friendly to blood sugar. These choices fit well into my eating plan.
- Berries like strawberries, blueberries, and raspberries are high in fiber and antioxidants with modest sugar.
- Apples offer fiber and water. A medium apple has about 19 grams of carbs and is filling.
- Pears provide fiber and potassium with about 10 grams of sugar per 100 grams.
- Peaches are a good snack with vitamin C and a gentle glucose impact.
- Kiwis bring vitamin C and fiber. I often pair sliced kiwi with plain yogurt.
- Oranges hydrate and supply vitamin C. I choose the whole fruit rather than juice.
- Plums taste sweet yet stay modest in sugar for a single fruit.
Whole fruits, not juices, offer more dietary fiber which slows sugar absorption[1]. This helps me satisfy a sweet tooth while keeping control.
Why select whole grains?
Whole grains like whole wheat, brown rice, barley, quinoa, and oats help manage blood sugar because fiber slows digestion. That means fewer sharp spikes after meals.
With the Plate Method, I usually set one quarter of my plate for whole grains or another quality carbohydrate. Fiber-rich choices can also lower blood pressure and support heart health, which matters for people with diabetes.
Many health care providers suggest starting with about half a cup of cooked brown rice or oatmeal per meal. Once I set whole grains, I turn to lean protein options to round out my plate.
What are the best lean protein options?
I rely on lean proteins to support fullness and steady energy. Chicken, turkey, and fish are strong picks. Heart-healthy fish like salmon, mackerel, tuna, and sardines give me omega-3 fats. I aim for two fish servings per week.
Beans, lentils, tofu, eggs, and nuts are excellent as well. I often use the Plate Method and make one quarter of my plate lean protein. This balance helps me manage hunger and glucose throughout the day.
How to incorporate healthy fats?
Healthy fats help my heart and make meals more satisfying. The right amount fits easily into a diabetes meal plan.
- I include avocados, nuts, and seeds for flavor and key nutrients.
- I cook with canola, olive, or peanut oil instead of butter or lard.
- I enjoy a small handful of almonds or walnuts for a snack, since portions matter due to calories.
- I eat omega-3 fish such as salmon, tuna, mackerel, or sardines at least twice per week.
- I spread natural nut butter on whole grain toast instead of sugary or high-fat spreads.
- I measure oils by the teaspoon to keep calories in check.
- I avoid foods with trans fats like packaged snacks and many fried items.
Adding healthy fats on purpose helps me feel satisfied and stick with my plan.
Which foods should be limited or avoided?
Some foods make blood sugar harder to control, so I choose carefully and plan ahead to protect my goals.
Why avoid sugary drinks and snacks?
Sugary drinks like regular soda, sweetened coffee, and fruit juice can raise blood sugar very quickly. Candy, cookies, and many cereals also carry a heavy dose of added sugar.
These choices cause rapid spikes, which can lead to health problems for people with diabetes. I set a daily limit for added sugar. The American Heart Association suggests no more than 25 grams for women and 36 grams for men. That simple target keeps me focused on better options.
How to cut back on refined carbohydrates?
Cutting refined carbs is one of the fastest ways I found to steady my glucose. Here are the steps I use.
- I swap white bread, pasta, tortillas, and white rice for whole grain versions.
- I choose brown rice, quinoa, or whole wheat bread at most meals.
- I limit fast food, sugary snacks, and convenience meals that pack refined carbs.
- I read ingredient lists and avoid items listing enriched or white flour first.
- I cook more at home to control how many carbs go into each dish.
- I switch sweet cereals for oatmeal or cereals with at least 3 grams of fiber per serving.
- I drink water or unsweetened beverages instead of soda or energy drinks.
- I use carb-counting tools or apps approved by my health care provider.
- I snack on nuts, seeds, berries, or cut vegetables instead of crackers or cookies.
- I check with a dietitian before trying any fad diet that promises fast results.
These habits help me avoid spikes and keep my numbers in range.
What are the risks of saturated and trans fats?
After trimming refined carbs, I review my fat choices. Saturated fats come from foods like butter, beef, sausage, bacon, full-fat dairy, and tropical oils like coconut and palm. Trans fats hide in many packaged snacks, baked goods, shortenings, and stick margarines.
Both can raise LDL cholesterol, which increases the risk of heart disease. People with diabetes face higher heart risks, so this step matters. Some past guidance set dietary cholesterol at under 200 milligrams per day. Today, experts still emphasize limiting saturated and trans fats to protect the heart.
Why limit processed meats?
Processed meats such as hot dogs, sausage, and bacon are high in saturated fat and sodium. Eating these often can raise blood pressure and strain the heart.
Research links processed meats with a higher risk of heart disease in people managing diabetes. I saw my glucose readings improve after I replaced sausage at breakfast with eggs, beans, or yogurt. Lean meats and plant proteins support steadier numbers and better health.
How to plan meals effectively for diabetes
Planning sets the pace for steady glucose. A simple framework makes daily meals easier and less stressful.
What is the diabetes plate method?
The diabetes plate method is a visual guide that helps me with portions and balance. I use a 9-inch plate. Half the plate is non-starchy vegetables like spinach, broccoli, or tomatoes. One quarter is a lean protein such as grilled chicken or tofu. The last quarter is a quality carbohydrate like brown rice, quinoa, or whole wheat pasta.
I add a small amount of healthy fat like olive oil or avocado. If my plan allows, I include a serving of fruit or dairy. For drinks, I pick water or unsweetened tea. This simple layout keeps my meals consistent and supports glucose control.
Why keep consistent meal times?
Consistent meal times help stabilize blood sugar. Regular meals support how insulin works in the body, whether from medicine or from my own pancreas.
Eating at set times reduces spikes and dips. For example, I feel best with breakfast at 7:00 AM, lunch around noon, and dinner at 6:00 PM. When I skipped lunch in the past, I felt shaky later. A schedule keeps energy steady and supports long-term health.
How can snacks help stabilize blood sugar?
Snacks can bridge the gap between meals and prevent low blood sugar. I pick snacks that include fiber, protein, or both. This slows digestion and keeps me steady.
Examples include whole grain crackers with nut butter, a small apple with cheese, Greek yogurt, nuts, or raw vegetables. I also match snack size to my blood sugar pattern and activity. That way, snacks help rather than hurt.
Popular diabetic diet approaches to consider
There is more than one way to build a healthy plate. These approaches can fit different tastes and cultures.
What are the benefits of a Mediterranean diet?
The Mediterranean diet highlights fruits, vegetables, whole grains, fish, olive oil, and nuts. Large studies report a lower risk of heart disease with this pattern. Healthy fats like extra virgin olive oil support better cholesterol and may reduce inflammation.
This approach limits processed foods and sugary snacks. It can improve glucose control compared with a diet high in refined carbs. When I shifted most meals to this style, my blood pressure improved within weeks.
How does a low-carb diet help diabetes?
A low-carb diet reduces how much glucose enters the blood after meals. Fewer carbs mean smaller rises in blood sugar. Carb counting helps people using insulin match doses more accurately.
Keeping my carbs steady at each meal made my diabetes easier to manage. Working with a dietitian helped me set goals that fit my lifestyle and medications.
What should you know about a plant-based diet?
Plant-based eating can also support glucose control. Research from respected institutions in 2023 showed that vegetarian patterns may lower blood sugar and improve cholesterol.
Beans, lentils, and tofu offer protein with little saturated fat. A plant-forward plate delivers more fiber, which improves fullness and supports heart health. When I swapped in bean chili or tofu stir-fry, my home glucose readings smoothed out.
| Food Group | Example Options | Recommended Servings |
|---|---|---|
| Non-starchy vegetables | Spinach, broccoli | Half plate |
| Whole grains | Brown rice, barley | Quarter plate |
| Lean plant proteins | Lentils, chickpeas | Quarter plate |
Careful planning ensures enough protein while keeping carbs balanced with fiber and healthy fats.
What are the benefits of following a diabetic diet?
Following a diabetes meal plan gives me more control over daily choices and health outcomes. Small changes build confidence and momentum.
How does it help control blood sugar?
A diabetic diet uses healthy carbs like fruits, vegetables, whole grains, legumes, and low-fat dairy. These foods release sugar more slowly into the blood. High-fiber options, such as whole fruits, beans, and oats, keep that rise even gentler.
Balanced meals also reduce sudden changes in glucose during the day. When I pick these foods and space meals well, my readings stay in range more often.
Can it reduce diabetes-related complications?
Good glucose control protects nerves, kidneys, eyes, and the heart. Studies show that smart meal patterns reduce the risk of kidney issues, nerve pain, vision loss, and heart problems.
Healthy eating can also prevent type 2 diabetes in some people with prediabetes. For me, choosing nutrient-dense foods has made checkups smoother and reduced worry over complications.
How does it support weight management?
Weight control adds another layer of protection. A diabetic diet focuses on nutrient-dense foods and portion control, which lowers calories without leaving me hungry.
Even a 5 to 10 percent weight loss can improve glucose and overall health, according to the American Diabetes Association. Vegetables, lean proteins, whole grains, and healthy fats help me feel satisfied. Regular meals reduce cravings and late-night snacking.
Why is it good for heart health?
Picking healthy fats like monounsaturated and polyunsaturated fats protects my heart. I use avocados, nuts, olive oil, canola oil, and peanut oil. Omega-3 fish such as salmon or tuna, eaten twice a week, add extra support.
Limiting saturated and trans fats lowers heart risk. Cutting sodium from processed foods helps manage blood pressure. These habits fit well with diabetes care and heart protection.
Why is monitoring blood sugar important?
Glucose checks turn guesswork into data I can use. Seeing patterns helps me adjust meals, activity, and medicine.
How often should you check glucose levels?
I check my blood glucose several times a day with a meter. I test before meals and after exercise to see how food and movement affect my numbers. The American Diabetes Association supports regular monitoring because many factors can change readings quickly.
Once, after a high-carb lunch, my meter showed a big spike. That feedback led me to adjust future lunches. ADA’s MyFoodAdvisor helps me log foods and match them with my results for better decisions.
How does diet maintain glucose stability?
Keeping carbs consistent at each meal helps my glucose stay in range. Carbohydrates raise blood sugar faster than protein or fat, so I measure portions using cups or a food scale.
Studies show that portion control and regular meal timing reduce spikes and crashes. High-fiber foods like whole grains, beans, non-starchy vegetables, and lean proteins slow digestion and smooth out changes in glucose.
Good planning supports my insulin response and reduces the risk of long-term issues. Careful eating makes the rest of diabetes management less stressful.
What are common mistakes in diabetes management?
Some habits make glucose control harder. I watch for these slip-ups and plan ahead to avoid them.
Why should you never skip meals?
Skipping meals can cause big swings in blood sugar. If I miss a meal, my glucose may drop too low, especially if I take insulin or other medicine.
Regular meals help insulin work better and keep energy stable. People who eat on a schedule have fewer highs and lows. The Plate Method makes planning those meals simple.
Can too much “healthy” food be harmful?
Overeating, even healthy food, can raise glucose and add extra calories. Foods like avocados, nuts, and olive oil are nutritious but energy dense.
My dietitian taught me to read serving sizes and daily values on labels. Paying attention to how much I eat is as important as what I eat.
Why pay attention to portion sizes?
Portion control protects against spikes. A common guide is 12 to 15 grams of carbohydrate per serving of starch, fruit, or milk.
Carb counting matters even more if you use insulin because dosage depends on carbs eaten. A registered dietitian can show how to read labels and build safe meal plans. Mastering portions helps me choose more non-starchy vegetables and nutrient-dense foods with confidence.
When should you seek help from a dietitian?
If your blood sugar feels hard to manage, a registered dietitian can help. Expert guidance turns medical advice into everyday steps that fit real life.
Why is professional advice necessary?
A registered dietitian or diabetes educator uses my medications, weight, other conditions, daily habits, and goals to suggest a plan that fits. They follow standards from the Academy of Nutrition and Dietetics and the Association of Diabetes Care and Education Specialists.
They teach key skills like portion control, label reading, and carb counting. Evidence-based coaching lowers complication risks by keeping glucose steadier.
How can meal plans be tailored to your needs?
Meal plans shift with medicine changes, weight goals, health conditions, schedule, taste, and culture. Dietitians use tools like ADA’s MyFoodAdvisor and clear handouts on carb counting and the glycemic index to guide choices.
After I adjusted my plan with a dietitian in 2022, my glucose became more stable. Clinical research also shows better outcomes when people follow personalized plans. Custom snacks and mealtimes can match work or family routines.
Conclusion
A thoughtful diabetic diet supports steady blood sugar, weight goals, and heart health. Daily choices, like whole grains, lean protein, non-starchy vegetables, and healthy fats, form a realistic meal plan that fits real life.
Working with a registered dietitian adds clear steps and ongoing support. With a plan that you can live with, managing diabetes becomes more consistent and far less stressful.
FAQs
1. What is a diabetic diet and why is it important for managing diabetes?
A diabetic meal plan helps control blood sugar by focusing on balanced meals with specific amounts of carbohydrates, protein, and healthy fats. Research shows that following such a plan can reduce the risk of complications like heart disease or nerve damage.
2. Which foods should people with diabetes avoid to manage their condition?
People living with diabetes should limit sugary drinks, processed snacks, white bread, and fried foods. Studies show these items can cause rapid spikes in blood glucose levels and may increase the risk of long-term health problems.
3. How does portion size affect blood sugar management in a diabetic diet?
Controlling portion sizes helps keep blood sugar stable throughout the day. For example, using smaller plates or measuring servings supports better glucose control according to clinical guidelines from leading medical organizations.
4. Can you share an example of how someone successfully managed diabetes through dietary changes?
One patient replaced sweetened beverages with water and chose whole grains over refined ones at each meal; after three months, her average daily glucose readings improved significantly as documented in her medical records.
Summary: A well-structured eating plan plays a key role in controlling diabetes by emphasizing nutrient-rich choices while limiting high-sugar foods. Evidence suggests that monitoring portions and making practical food swaps leads to better health outcomes for those managing this condition.