Unlock The Benefits Of Nutrition Therapy And Medical Nutrition Therapy
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
If you are managing a medical condition like diabetes or high cholesterol, food choices can feel confusing. Nutrition therapy uses science-based steps to guide your meals and support your health. With a clear plan and steady support, you can eat with confidence and feel better day to day.
In this guide, you will see how nutrition therapy and medical nutrition therapy work, what benefits they bring, and how a registered dietitian builds a plan that fits your life. You will also learn simple actions that move you toward better health without guesswork.
Small changes matter. A few smart swaps, practiced daily, can add up to real results.
Key Takeaways
- Nutrition therapy and medical nutrition therapy, called MNT, use personalized plans from registered dietitian nutritionists to manage diabetes, heart disease, kidney disease, and digestive conditions.
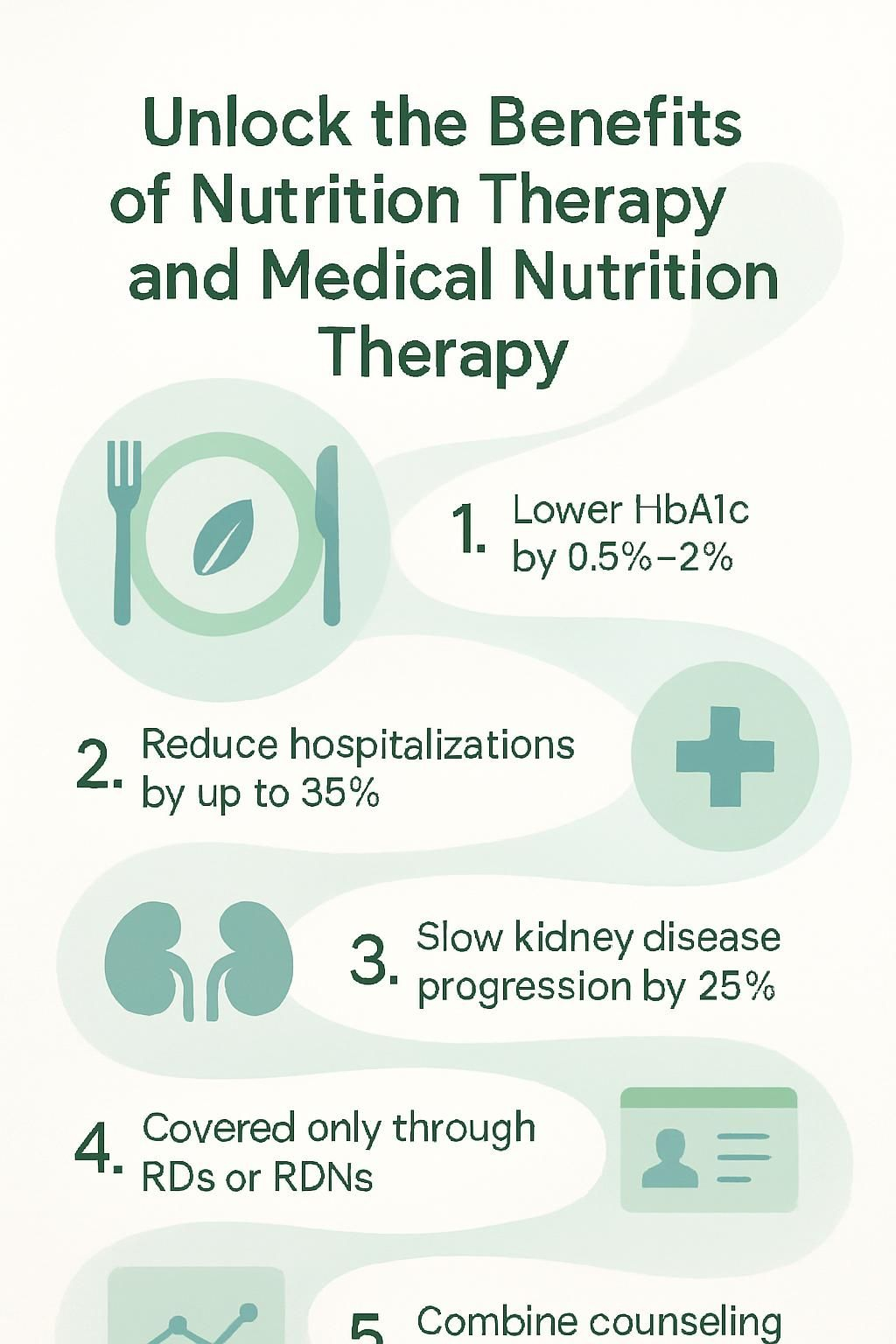
- Evidence shows MNT can lower HbA1c by about 0.5 to 2 points, cut hospitalizations for diabetes and heart failure by up to 30 percent, and slow chronic kidney disease by roughly 25 percent.
- Only RDs or RDNs with approved training can deliver MNT that Medicare or other insurance covers in the United States. The title nutritionist is not regulated.
- Progress checks through lab results and follow-up visits allow adjustments over time, using trusted guidance from sources like the Academy of Nutrition and Dietetics.
- Behavior counseling plus diet changes helps remove barriers and supports lasting weight loss, which can improve cholesterol, blood sugar, and long-term outcomes.
What Is Nutrition Therapy?

Nutrition therapy uses food and nutrition to support health and treat diet-related issues. A nutrition professional, often a registered dietitian nutritionist, creates a plan that matches your medical needs, lifestyle, and goals.
What does nutrition therapy mean and what is its purpose?
Nutrition therapy is a structured, food-based treatment that helps prevent and manage many conditions. You work with a trained expert who uses proven methods, then shapes those methods into a plan that fits your life.
Common goals include lowering blood sugar in diabetes, improving cholesterol and triglycerides, easing digestive symptoms, and supporting healthy weight. Education is part of care, so you learn meal planning, label reading, and simple ways to build better habits.
This work respects your culture, preferences, and routine. Plans also address real-world barriers like limited time or food access. The aim is a healthy relationship with food while managing issues such as type 2 diabetes, heart disease, or irritable bowel syndrome, called IBS.
An effective plan has several moving parts. Knowing these parts will help you get the most from your visits.
What are the key components of nutrition therapy?
Care starts with a full nutrition assessment. Your provider reviews your diagnoses, labs, medications, eating patterns, allergies, symptoms, and daily habits. That snapshot reveals risks, strengths, and nutrient gaps.
Personalization is central. Your plan may adjust portion sizes, swap certain foods, or include supplements when needed. Some medical situations require advanced support like tube feeding, called enteral nutrition, or IV feeding, called parenteral nutrition.
For example, people with kidney disease often need to limit sodium and potassium. Those with high triglycerides may increase fiber and reduce added sugars.
Follow-up visits track results and fine-tune the plan. Education and small, steady changes build skills you can keep using. This model supports diabetes, kidney disease, and gastrointestinal disorders such as Crohn’s disease and ulcerative colitis.
What Is Medical Nutrition Therapy (MNT)?
Medical nutrition therapy is a clinical service that treats and manages medical conditions with a personalized nutrition plan. A registered dietitian nutritionist partners with your medical team to align food choices, medications, and lab goals.
What is medical nutrition therapy?
Medical nutrition therapy is individualized nutrition care for a specific diagnosis. Your dietitian reviews your history, labs, medicines, and lifestyle, then builds a plan to match your medical needs.
That plan may include nutrition education and targeted diet changes. If you cannot swallow or digest well, it can include tube feeding or IV nutrition to deliver nutrients safely.
Dietitians coordinate with your doctors and set measurable goals for conditions like type 1 diabetes, chronic kidney disease, Crohn’s disease, celiac disease, and dyslipidemia, which means unhealthy cholesterol or triglycerides. Care takes place in hospitals, outpatient clinics, or through insurance-covered visits, including Medicare in the United States.
This is an ongoing process that aims to improve symptoms, lab values, and quality of life over time.
How does nutrition therapy differ from medical nutrition therapy?
Nutrition therapy can offer general wellness guidance and basic food education. In the United States, anyone may call themselves a nutritionist, since the term is not regulated.
Medical nutrition therapy is different. It must be delivered by an RD or RDN with specialized clinical training and, in many states, a license. MNT follows medical protocols and addresses diagnosed conditions like diabetes, kidney disease, heart disease, or Crohn’s disease.
Medicare and most insurers reimburse MNT only when provided by an RD or RDN. In my own kidney transplant recovery, work with a registered dietitian included lab review, a structured meal plan based on Academy of Nutrition and Dietetics guidelines, and regular follow-ups. It felt far more precise than past visits with general nutrition coaches.
How Nutrition Therapy Works
Nutrition therapy follows a clear path, from assessment to action. The plan is personal, but the process is consistent.
How is nutritional status assessed?
Your assessment maps the road ahead. A dietitian gathers information to create an accurate nutrition diagnosis and plan.
- Share your medical history, current medications, surgeries, and past illnesses such as kidney transplant or Crohn’s disease.
- Explain your food preferences, allergies, and any barriers to healthy choices, including cost or limited access.
- Describe your activity level, work schedule, sleep, and stress patterns, since these influence energy needs.
- Complete lab tests like fasting glucose or cholesterol. Objective numbers guide safe, evidence-based care.
- Discuss cultural or personal values around eating so your plan respects your background.
- Report symptoms such as constipation, heartburn, or pain, which may signal changes needed in your diet.
- Bring referral notes from your physician to support coordinated care that includes medical nutrition therapy.
How are personalized nutrition plans developed?
Once the assessment is complete, your dietitian designs a step-by-step plan that matches your goals and health data.
- The RD reviews your medical history, labs, and food recall to spot nutrition-related problems and nutrient gaps.
- A nutrition diagnosis is made. It might include high LDL cholesterol, poor blood sugar control, or low iron.
- Measurable targets are set, for example lowering LDL by 10 percent in three months or reducing A1C to a safer range.
- Action steps are outlined, such as adjusting carbohydrates for blood sugar control or adding fiber to support digestion.
- You receive a detailed plan with meal ideas, portion sizes, nutrient goals, and simple shopping tips.
- During the session, you discuss cooking methods, eating frequency, and habits that influence results.
- Telehealth can extend support between visits, which is helpful during dialysis or Crohn’s disease flares.
- Apps may help track food and symptoms. Some plans may consider genetics for extra personalization.
- Your role is active. Follow the plan and share honest feedback during check-ins.
- Many clients reach goals like weight loss or better lab results with clear steps and steady coaching.
Every step uses current research and, when relevant, Medicare guidance to keep care safe and effective.
How are dietary and lifestyle changes implemented?
Change works best in small, doable steps. Your dietitian turns goals into daily actions you can repeat.
- They review food diaries, history, and labs to understand your starting point.
- Together you agree on a plan that fits your condition and preferences, such as diabetes or Crohn’s disease.
- Education happens in 1-on-1, group, or telehealth sessions to build skills and remove barriers.
- Plans often include limiting some foods, increasing nutrient-dense choices, and using supplements when needed.
- Activity goals support cholesterol, weight, and blood sugar improvements.
- Practical tips cover grocery lists, fast prep ideas, and dining out strategies.
- Regular monitoring checks progress and guides adjustments using evidence-based tools.
- Apps or wearables can track intake, activity, and health markers in real time.
- Ongoing feedback from your RDN keeps the plan effective for the long run.
How Medical Nutrition Therapy Works
MNT follows a structured, clinical process led by a registered dietitian. Think of it as nutrition care that connects your plate to your lab results.
What is the role of a Registered Dietitian Nutritionist (RDN) in MNT?
An RDN designs and manages your plan using current science and clinical standards. They coordinate with your healthcare team so nutrition aligns with your diagnosis and medicines.
Dietitians apply evidence-based guidelines for diabetes, kidney disease, and Crohn’s disease. They teach, coach behavior change, and adjust your plan during follow-ups. This teamwork helps you digest foods better, meet nutrient needs, and support medical treatments from your doctor.
What evidence-based interventions are used for chronic conditions?
After the plan is set, your dietitian uses proven interventions. Food changes are the core strategy for most conditions.
For diabetes, common steps include carbohydrate counting and limiting added sugars. In chronic kidney disease, protein, phosphorus, potassium, and sodium often need close control. For heart failure, sodium and fluid limits help lower strain on the heart.
Some people need tube feeding or IV nutrition when eating is not safe. Supplements can fill gaps when food alone is not enough. For Crohn’s disease, plans may shift during flare-ups, for example using lower fiber and adding omega-3s to support gut health.
Research shows targeted MNT can reduce hospital admissions by up to 30 percent for conditions like heart failure and diabetes complications. Results are tracked with labs and check-ins so you can see steady improvement over time.
…
[1] American Diabetes Association, Standards of Care in Diabetes 2024; Journal of Renal Nutrition 2018; Academy of Nutrition and Dietetics, Evidence Analysis Library
How is progress monitored and what happens during follow-up visits?
Follow-ups keep your plan fresh and safe. Each visit reviews data, then sets the next steps.
- Your dietitian reviews new labs, such as A1C or cholesterol, and compares them to your goals.
- You discuss any challenges, symptoms, or changes in routine that affected your plan.
- Questions about specific conditions, such as Crohn’s disease or kidney health, are addressed directly.
- Food records, weight trends, and patterns are checked for progress.
- Simple charts or checklists show what is improving and what needs attention.
- Barriers are identified, and solutions are chosen together.
- The plan is adjusted to match your current health markers and feedback.
- You leave with clear action steps and a date for the next check-in.
- Regular contact builds momentum and accountability for long-term success.
Benefits of Nutrition Therapy
With the right plan, nutrition therapy improves key numbers, eases symptoms, and prevents complications. The goal is steady progress you can sustain.
How does nutrition therapy improve health markers like cholesterol and blood sugar?
Targeted food choices can lower cholesterol and stabilize blood sugar. Plans often highlight whole grains, lean proteins, vegetables, fruits, and healthy fats.
Reducing saturated fat can drop LDL cholesterol by up to 10 percent in six weeks. Fiber slows the absorption of sugar, which helps prevent spikes and dips through the day.
People who receive regular nutrition counseling reach goals more often than those who only see a primary care provider. Progress is tracked through labs so you and your care team can adjust quickly.
How does nutrition therapy help manage chronic conditions?
Many chronic conditions respond well to consistent nutrition care. Diabetes, kidney disease, and heart failure are major examples.
For diabetes, plans guide carbohydrate amounts and timing. For heart disease, strategies reduce salt and saturated fat. In some cases, strong nutrition care decreases the need for certain medicines, though you should always follow your doctor’s advice.
Registered dietitians match recommendations to your health history and challenges. Regular check-ins support safe changes and better quality of life.
How does nutrition therapy prevent complications?
A balanced plan helps control risk factors that lead to complications. Structured meal timing and smart food choices can prevent blood sugar spikes and support steady energy.
Studies show that nutrition therapy can reduce hospital stays related to diabetes and heart disease by up to 30 percent, based on American Diabetes Association reports. Activity, stress management, and follow-up visits strengthen results and protect long-term health.
Simple swaps, like choosing whole grains instead of refined grains, can improve cholesterol without adding medicine. Many small improvements add up over time.
Benefits of Medical Nutrition Therapy
MNT turns science into a plan you can use every day. With an RDN’s guidance, you can target the outcomes that matter most to you.
How does MNT support diabetes management?
MNT for diabetes focuses on keeping blood glucose within a safe range. Dietitians often use carbohydrate counting and portion control, then combine those strategies with your medicine plan.
Research shows MNT can lower HbA1c by about 0.5 to 2 points for people with type 1 or type 2 diabetes. Some people need fewer medicines as their numbers improve, though medical decisions should always be made with your physician.
Plans adapt as labs and symptoms change. That flexibility keeps care relevant and effective.
How does MNT help with kidney disease and digestive disorders?
For chronic kidney disease, MNT manages protein, sodium, potassium, phosphorus, and fluids to reduce stress on the kidneys. Careful changes can control swelling and blood pressure. Many programs show slower disease progression and better quality of life.
Digestive conditions such as celiac disease, Crohn’s disease, IBS, and ulcerative colitis often need long-term nutrition support. An RDN can adjust fiber, lactose, and other triggers to reduce pain and prevent malnutrition. I worked with a dietitian for IBS, and a few fiber changes eased daily discomfort within weeks.
How does MNT aid in weight management and cardiovascular health?
MNT helps you build habits that support a healthier weight. Plans usually feature real foods, balanced portions, and gradual changes that stick.
For heart health, MNT targets blood pressure and lipids. Reducing sodium and saturated fat, while increasing fruits, vegetables, and healthy fats, can lower risk and improve cholesterol and triglycerides. Personalized steps make it practical to follow.
Key Conditions Treated By Nutrition Therapy
Nutrition therapy supports many diagnoses with clear, personalized steps. This targeted approach can improve lab values and daily comfort.
How does nutrition therapy address Type 1 and Type 2 diabetes?
For type 1 diabetes, you match insulin with carbohydrate intake at meals and snacks. This improves control and reduces highs and lows.
For type 2 diabetes, priority areas include balanced meals, portion control, and steady activity. These changes support weight loss and better blood sugar. Healthcare teams use these methods for prediabetes and gestational diabetes as well.
The Centers for Disease Control reports that effective nutrition therapy can improve HbA1c by up to 2 percent in type 2 diabetes^1^. Goal setting keeps the plan realistic and personal.
…
^1^ CDC: Diabetes Self-Management Education and Support, DSMES Toolkit
How is heart disease managed with nutrition therapy?
Nutrition therapy addresses heart failure, high blood pressure, and unhealthy lipid levels. A registered dietitian creates a plan that favors fruits, vegetables, whole grains, and unsaturated fats while limiting sodium and processed foods.
Improved eating patterns can lower blood pressure, LDL cholesterol, and triglycerides. Some people need fewer medications over time, based on their doctor’s guidance. In my own case, swapping salty snacks for fresh produce improved energy and blood pressure within weeks.
How does nutrition therapy help gastrointestinal disorders like Crohn’s and IBS?
For Crohn’s disease and IBS, nutrition therapy can reduce symptoms by identifying and limiting trigger foods. Plans often include smaller meals, careful fiber adjustments, and support to prevent nutrient shortfalls like vitamin B12 deficiency.
Working closely with a dietitian makes it easier to manage flares and maintain weight. A few practical shifts can bring noticeable relief.
How does nutrition therapy support kidney disease treatment?
Nutrition therapy helps protect kidney function at every stage of chronic kidney disease. Plans guide sodium, potassium, phosphorus, and protein to reduce strain on the kidneys.
Many people with CKD aim for sodium under 2,300 milligrams per day. Fluids and supplements are adjusted based on labs. In advanced disease or during dialysis, tube feeding may be needed if oral intake is not enough.
Family experience showed me that a focused plan can ease swelling and boost energy. Research in Kidney International reports that medical nutrition therapy may slow kidney decline by about 25 percent over one year compared with usual care alone.
Role of Nutrition Therapy in Weight Loss
Nutrition therapy can simplify weight loss with structure, coaching, and accountability. The aim is progress you can keep.
How does behavioral counseling support sustainable weight loss?
Behavioral counseling gives you tools to build new habits and stick with them. Together you set realistic goals, track progress, and practice skills like mindful eating and meal planning.
Many people struggle with stress eating or dips in motivation. Counseling sessions help you spot triggers and choose better responses. Working with an RDN helped me replace stress snacking with short walks and protein-rich snacks, which kept me on track.
What are common barriers to healthy eating and how can they be addressed?
Life gets busy, and barriers can slow your progress. A good plan meets you where you are.
- Limited access: Explore budget-friendly choices, food pantries, and farmer’s markets to expand options.
- Time pressure: Use short recipes, batch cooking, and simple snack packs to save time.
- Taste and culture: Keep familiar flavors and traditions while tweaking portions or cooking methods.
- Unhelpful habits: Learn mindful eating and set regular meal times to prevent overeating.
- Knowledge gaps: Practice reading labels and measuring portions to guide smarter choices.
- Personal obstacles: Share challenges during visits so your plan can adjust to your needs.
- Social pressure: Plan for dining out, parties, and work events without losing momentum.
- Chronic conditions: Make sure strategies fit your diagnosis and medicine schedule.
- Motivation dips: Use check-ins and tracking tools to spot problems early and reset goals.
What strategies support long-term weight maintenance?
Keeping weight off is a skill you can learn. These strategies help you protect your progress.
- Track meals and snacks to notice patterns and triggers that influence choices.
- Set specific goals that match your routine and time, then review them monthly.
- Work with an RDN to keep the plan personal and practical.
- Stay engaged with regular follow-ups. Support improves long-term success rates.
- Adjust your plan as life changes. Small updates prevent backsliding.
- Make gradual shifts that you can stick with rather than extreme rules.
- Prepare for barriers with backup plans, like freezer meals and healthy snacks.
- Lean on friends, family, or groups for encouragement and accountability.
- Use simple apps or trackers to watch trends and celebrate wins.
With these tools in place, you can move into newer options like telehealth, apps, and genetics to refine your plan even more.
Advances in Nutrition Therapy
New tools make care more flexible. Technology can help you get support at the right time and place.
How is telehealth used in nutrition therapy?
Telehealth lets you meet with a dietitian online for coaching, check-ins, and quick questions. It is helpful if travel is hard or your schedule is tight.
Video or secure chat visits make it easy to review labs, adjust goals, and solve meal planning issues between in-person appointments. Virtual visits saved me hours during a busy school season, yet my progress stayed on track.
How is technology integrated into nutrition monitoring and planning?
Digital tools let you log food, activity, and symptoms in minutes. Photo logs and barcodes speed tracking and improve accuracy.
Apps like MyFitnessPal can track calories and nutrients, then highlight trends. That information helps you and your dietitian update your plan using real data, not guesswork. When I tracked meals after my doctor suggested nutrition therapy, small changes felt rewarding because the app showed quick wins.
How does genetic information personalize nutrition therapy?
Genetic reports can explain how you process nutrients like fat, carbs, and vitamins. Some people absorb vitamin D poorly, while others may be salt sensitive, which can affect blood pressure.
With this insight, your dietitian can fine-tune targets and food choices. Studies in 2022 found that nutrition plans informed by genetics improved weight loss and blood sugar in adults with prediabetes.[1] For me, using family history as a guide made each suggestion feel relevant and doable.
A short summary: genetic data can sharpen your plan and support better results.
…
[1] Nutrigenomics and Personalized Nutrition, Advances in Nutrition, 2022
Choosing the Right Nutrition Therapy Provider
The right expert makes change easier. A qualified professional creates a plan that fits your health and your everyday life.
Why is it important to work with a licensed dietitian?
Licensed dietitians have the training to deliver safe, effective medical nutrition therapy. Only RDs or RDNs can provide MNT that Medicare or other insurers cover.
These professionals manage complex conditions, interpret labs, and adjust plans as your health shifts. If you want care based on strong evidence rather than trends, a dietitian is your best bet.
What questions should you ask your nutrition therapy provider?
Good questions lead to better care. Use these to find the right fit.
- Can you share your RD or RDN credentials and your experience with my condition?
- How will you build a plan that matches my medical needs, routine, and preferences?
- How often do we meet, and how will you track my progress?
- Which evidence-based methods do you use for diabetes, heart disease, or kidney disease?
- What is your process for adjusting the plan if I am struggling?
- Do you accept my insurance, and can you provide documentation for coverage?
- Will you coordinate with my physician or specialist if needed?
- How do you stay current with new nutrition research and apply it to care?
These questions help you choose someone who can deliver the support you need.
How can you verify credentials and specialization?
Check credentials before your first visit. This protects your health and your budget.
- Look for RD or RDN after the provider’s name to confirm professional training.
- Use your state licensing board website to confirm active licensure.
- Search the Academy of Nutrition and Dietetics Find an Expert directory for membership and specialties.
- Ask about training in MNT or focus areas like diabetes, kidney care, heart health, or digestive disorders.
- Request proof of continuing education, which dietitians must complete regularly.
- Verify completion of an ACEND-accredited supervised practice program.
- Review any research, articles, or presentations the provider has authored.
- Make sure recommendations are personal and evidence-based, not generic advice or untested supplements.
- Confirm with your insurer that your provider’s credentials meet coverage rules.
- Avoid services from anyone using the title nutritionist without recognized registration or state licensure.
Potential Risks of Medical Nutrition Therapy
MNT is safe when guided by a qualified professional. Managing complex conditions without expert support can create risks.
What are the risks of mismanaging conditions with MNT?
Without clinical guidance, you could develop nutrient deficiencies or consume harmful amounts of certain nutrients. For example, excess sodium can raise blood pressure and strain the kidneys.
Improper use of IV nutrition or tube feeding raises the risk of infection, fluid or electrolyte problems, and even organ damage. Close supervision by a registered dietitian protects you from these issues.
Why is professional guidance important in MNT?
IV feeding can cause bloodstream infections if not managed correctly. Tube feeding can lead to site infections, nausea, diarrhea, or constipation.
A registered dietitian monitors labs, symptoms, and tolerance, then adjusts your plan as needed. This oversight keeps changes safe and matched to your medical needs.
How to Prepare for Nutrition Therapy
A little prep work makes your first visit count. Gather key details so your plan starts strong.
What medical history and lab results should you gather?
Bring a clear list of diagnoses, surgeries, hospital stays, and current medicines or supplements. Include conditions like diabetes, kidney disease, or heart issues.
Collect recent labs such as fasting glucose, A1C, lipid panel, iron studies, vitamin D, and kidney function tests. These numbers help your dietitian build a plan that matches your needs. I brought my medication list and labs to my first visit, and it sped up the process.
How do you set realistic health goals?
Work with your dietitian to set goals that are specific and doable. Aim for outcomes you can measure within a set time frame.
For example, lower fasting glucose by 10 mg/dL in three months, or increase vegetables to two cups per day. One of my clients chose a goal of losing five pounds in eight weeks, which felt reasonable and motivating.
How can you prepare for lifestyle changes?
Share any limits around time, budget, or food access. That honesty helps your dietitian build a plan that fits your life.
Keep a simple food and drink log for a week. Patterns become clearer on paper, and that makes the first changes easier. Studies on patient-centered care show that practical plans lead to better long-term results.
FAQs About Nutrition Therapy
Here are direct answers to common questions. Use them to plan your next steps with confidence.
What is artificial nutrition?
Healthcare teams use two terms for what many call artificial nutrition. Parenteral nutrition delivers nutrients through an IV. Enteral nutrition delivers liquid food through a tube into the stomach or intestine.
These methods are used when swallowing or digestion is unsafe, such as after surgery. During my own hospital stay after throat surgery, a feeding tube kept me nourished while I healed. Dietitians guide these therapies as part of medical nutrition therapy.
How long does nutrition therapy usually last?
The length of care depends on your condition and goals. Some plans last a few months, while others continue for years for chronic issues like diabetes.
Frequency often changes as you improve. My visits began weekly, then moved to monthly after three months as my labs improved. Regular check-ins help sustain gains in cholesterol, blood sugar, and weight.
Is nutrition therapy covered by insurance?
Many insurance plans cover medical nutrition therapy when delivered by an RD or RDN. Medicare Part B covers MNT for diabetes and kidney disease in the United States when provided by a qualified dietitian.
Coverage varies, so call your insurer before booking. A quick call saved me surprise costs when I sought help for high cholesterol.
Next, find out what medical nutrition therapy is and how it differs from standard nutrition care.
Conclusion
Nutrition therapy and medical nutrition therapy can guide you through real change. With a registered dietitian, you get a plan that fits your health needs and daily life.
These services help manage diabetes, kidney disease, and heart conditions, and they can improve lab values like cholesterol and blood sugar. With a personal plan, healthy habits become easier to maintain.
This article is educational and does not replace medical advice. Talk with your physician and a registered dietitian before making major changes, especially if you have a chronic condition or take prescription medicine.
FAQs
1. What is nutrition therapy and how does it help?
Nutrition therapy uses a plan tailored to your individual needs. It helps manage health conditions by improving eating habits and nutrient intake. Research shows that personalized plans can lower blood sugar, cholesterol, and blood pressure in people with chronic diseases such as diabetes or heart disease (Academy of Nutrition and Dietetics, 2022).
2. How is medical nutrition therapy different from general nutrition advice?
Medical nutrition therapy involves a registered dietitian who creates a plan tailored to your individual needs based on medical history, lab results, and lifestyle factors. This approach relies on clinical evidence to address specific health problems rather than offering broad dietary tips.
3. Who should consider a plan tailored to their individual needs through medical nutrition therapy?
People with chronic illnesses like kidney disease or diabetes benefit most from this type of care. For example, after my diagnosis of prediabetes last year, my doctor referred me for medical nutrition therapy; the dietitian designed meals that fit both my preferences and health goals.
4. What are the main benefits of having a plan tailored to your individual needs in nutrition therapy?
A personalized approach improves treatment outcomes because it addresses unique challenges such as allergies or medication side effects. Studies show patients following individualized plans have better long-term success managing weight and symptoms compared to those using generic diets (Journal of Clinical Nutrition, 2021).
Summary: Nutrition therapy offers targeted support by creating plans suited for each person’s situation; this leads to improved management of many health issues when compared with one-size-fits-all advice.







