Nutrition During Pregnancy: Essential Diet For Pregnant Women
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
Sorting through advice can feel overwhelming. Still, smart nutrition during pregnancy gives your body, and your baby, what they need most. A healthy diet adds key nutrients and the right calories to support growth and steady energy.
This guide explains the essentials, from vitamins and minerals to safe food choices. You will also find simple tips for meals, snacks, and hydration through every trimester.
Key Takeaways
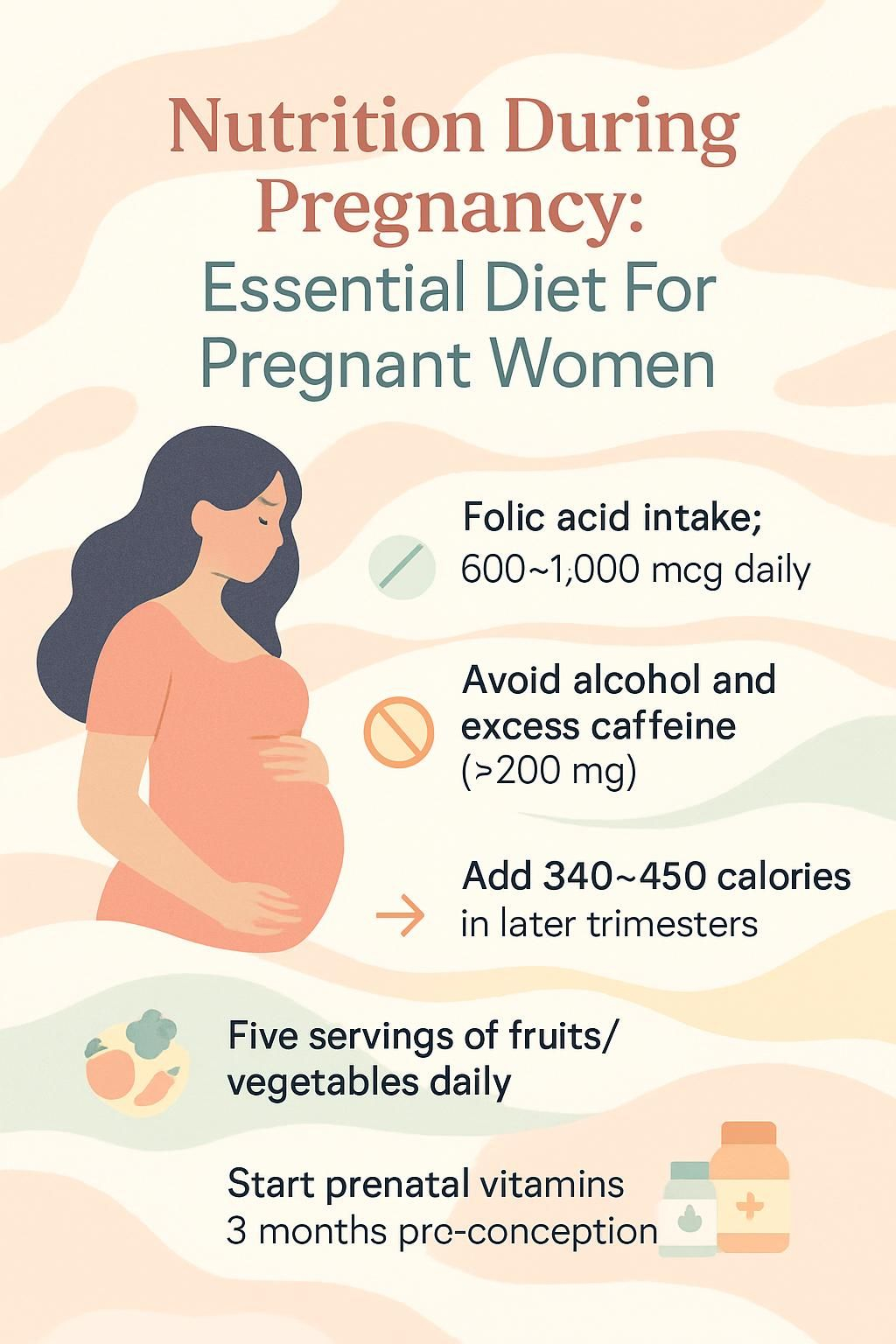
- Daily targets support fetal development: folic acid 600–1,000 mcg, iron 27 mg, calcium 1,000 mg, vitamin D 600 IU, protein 71 grams.
- Avoid raw or undercooked meat, unpasteurized dairy, high‑mercury fish like shark, swordfish, and marlin, alcohol, and excess caffeine over 200 mg per day.
- Public health guidance suggests at least five servings of fruits and vegetables daily, plus whole grains, lean proteins, dairy or fortified alternatives, nuts, seeds, beans, and peas.
- Calorie needs rise with each trimester: first, no extra; second, about +340 per day; third, about +450 per day.
- Begin a prenatal vitamin with at least 400 mcg folic acid and 27 mg iron, ideally three months before conception, to lower neural tube defect risk.
The Importance of Nutrition During Pregnancy

Food choices shape your health, your baby’s growth, and pregnancy outcomes. A healthy diet sets a strong foundation for both of you.
How does nutrition affect the health of mother and baby?
Eating balanced meals with protein, fruits, vegetables, and whole grains supplies the vitamins and minerals needed for development. Good nutrition helps prevent birth defects of the brain and spine, called neural tube defects. It also supports steady weight gain and a healthy placenta.
Iron supports blood production for you and your baby, lowering the risk of anemia. A balanced pattern reduces complications like preterm birth and high blood pressure. Experts from the U.S. Department of Health and Human Services note that variety across food groups improves outcomes for pregnant women and infants.
High quality foods aid fetal growth, bone and tooth formation, and mood after delivery. During my first trimester, small meals with leafy greens eased nausea and helped me stay on track with weight gain recommended by my midwife.
Every bite counts when growing a new life; healthy food choices matter for every stage of pregnancy.
What role does a balanced diet play in pregnancy outcomes?
A balanced diet fuels growth, supports your immune system, and helps you feel well. Aim for fruits, vegetables, whole grains like oats and brown rice, lean proteins such as poultry and beans, and healthy fats from nuts and seeds.
About one third of your intake can come from starchy foods like whole wheat bread, potatoes, and pasta for steady energy. This variety delivers folic acid, calcium, iron, and vitamin D, which work together to prevent neural tube defects, build bones, support blood, and protect the heart.
Include at least five servings of fruits and vegetables each day. This pattern supports digestion, reduces constipation, and provides antioxidants that help protect cells. Limiting added sugars and unhealthy fats helps manage weight gain during pregnancy and supports heart health.
Safe dairy, like yogurt and hard cheese, plus iron‑rich foods such as beans and lean beef, can help prevent anemia. Following the Dietary Guidelines for Americans, with input from your healthcare professional, improves your chance of a healthy pregnancy and smoother recovery after birth.
Key Nutrients for Pregnant Women
Nutrient needs rise during pregnancy to support rapid growth and organ development. Food comes first, and a prenatal vitamin can help fill gaps.
Why is folic acid important for preventing neural tube defects?
Folic acid, the supplemental form of folate, protects babies from neural tube defects that affect the brain and spine. The U.S. Public Health Service advises 400 mcg daily for all who may become pregnant. During pregnancy, needs rise to 600–1,000 mcg.
These defects form early, often within 28 days of conception, which is why an early start matters. Fortified breakfast cereals and leafy greens help raise intake. Many people also rely on a prenatal vitamin to reach the daily goal, especially before pregnancy.
Some may need higher doses, for example those taking certain seizure medicines. Talk with your clinician for personalized advice.
“The right nutrients at the right time make all the difference for mother and baby.”
Include folate‑rich foods daily. Diet alone can fall short on busy days, so consistent habits are key.
How does iron support blood production and prevent anemia?
Iron helps your body make hemoglobin, the protein in red blood cells that carries oxygen to your organs and your baby. During pregnancy, the daily target is 27 mg. Low iron can cause tiredness, infections, preterm birth, and a higher risk of postpartum depression.
Choose iron‑rich foods such as fortified hot cereals, beans and peas, leafy greens, and lean beef. Pair plant iron with vitamin C foods like oranges or tomatoes to improve absorption. This steady approach helps prevent anemia and supports healthy growth.
What benefits does calcium provide for bones and teeth?
Calcium builds strong bones and teeth for your baby and protects your own bones. If your diet falls short, your body will draw calcium from your bones to supply the fetus. Pregnant adults need 1,000 mg per day, and pregnant teens need 1,300 mg.
Calcium also supports muscles, nerves, and blood vessel function. Good options include fortified orange juice, low‑fat cheese, yogurt, and milk or calcium‑fortified soymilk. During my first pregnancy, fortified soy milk helped me meet my goal when dairy felt hard to tolerate.
Regular intake creates a strong base for lifelong bone and dental health for both of you.
How does vitamin D enhance calcium absorption and bone health?
Vitamin D helps your gut absorb calcium, which strengthens bones and teeth for you and your baby. The target during pregnancy is 600 IU daily. A 3‑ounce serving of cooked salmon provides about 570 IU. A cup of skim milk offers around 100 IU.
Fortified cereals and eggs also contribute. Many people notice fewer cramps and steadier energy after meeting vitamin D needs. Meeting this goal helps prevent bone weakness and supports overall growth.
Why is protein essential for growth and development?
Protein builds cells, hormones, muscles, and skin. Pregnant women need about 71 grams daily. This supports your baby’s organs and your changing body.
Helpful sources include eggs, beans, fish low in mercury, poultry, yogurt, cottage cheese, and tofu. One cup of low‑fat cottage cheese has about 28 grams. A 3‑ounce portion of chicken gives around 26 grams. Adding eggs or beans at breakfast kept me full and steady through the morning.
How do omega-3 fatty acids boost brain and eye development?
Omega‑3 fatty acids, especially DHA, support brain and eye development. Fish like salmon, herring, trout, sardines, and pollock are rich in DHA. Eating two portions of fish weekly, with at least one oily fish, is linked with better infant vision and attention.
The body does not make much DHA, so food or a prenatal supplement matters. Including low‑mercury fish helps both your heart and your baby’s nervous system.
How does fiber help prevent constipation during pregnancy?
Fiber supports digestion and regular bowel movements. Hormone shifts can slow the gut during pregnancy, which raises the risk of constipation. Aim for 25 to 30 grams of fiber daily from fruits, vegetables, whole grains, beans, nuts, and seeds.
Drink water with fiber to keep stool soft. Many pregnant women feel relief after adding oatmeal, berries, and leafy greens to meals. Next, see which foods to prioritize in your daily plan.
Ideal Foods to Eat During Pregnancy
Focus on variety. Different colors and food groups deliver different nutrients your baby needs.
What fruits and vegetables are best to eat during pregnancy?
Choose colorful produce each day. Carrots, sweet potatoes, pumpkin, spinach, cooked greens, tomatoes, and red peppers deliver vitamin A and potassium. These support vision, immune health, and fluid balance.
Cantaloupe, melons, mangoes, prunes, bananas, apricots, oranges, and grapefruit are great fruit options rich in potassium and fiber. Citrus also boosts iron absorption from beans and greens.
Wash produce well to lower the risk of food poisoning. High fiber vegetables ease constipation, a common concern. Following MyPlate guidance to eat a rainbow across the week supports your energy and your baby’s growth.
Why are whole grains important during pregnancy?
Whole grains provide B vitamins, iron, fiber, and folic acid. These nutrients support blood production and reduce constipation. Make space for whole grain bread, brown rice, oatmeal, quinoa, and whole wheat pasta.
Starchy foods can make up about one third of your intake, with whole grain choices for longer lasting energy. Switching to whole grain toast and brown rice often reduces cravings and afternoon slumps.
What lean proteins are safe and healthy for pregnant women?
Lean proteins build tissue and support your immune system. Beans, peas, nuts, and seeds offer protein, fiber, and minerals. Well‑cooked beef, pork, and lamb are safe choices when cooked until no pink remains.
Choose low‑mercury fish such as salmon, trout, herring, sardines, and pollock to gain omega‑3s. I added more legumes during pregnancy to meet my needs while keeping meals interesting. Always cook meat and poultry thoroughly to reduce the risk of harmful bacteria.
Which dairy products support pregnancy nutrition?
Fat‑free or low‑fat yogurt, milk, and cheese provide calcium, protein, and vitamin D. Fortified soymilk is a good dairy alternative with similar nutrients. Aim for three servings a day to support bones and teeth.
Many find yogurt easier to digest, especially with lactose intolerance. Low‑fat cheese can be a steady snack when morning sickness makes large meals tough.
How do legumes and beans benefit pregnant women?
Beans and lentils are powerhouses for protein, fiber, iron, and folate. These nutrients support blood production and help prevent anemia. Fiber also eases constipation.
Try black beans, kidney beans, or chickpeas in salads, tacos, and soups. During my pregnancy, lentil soup made it easy to meet protein goals without meat at every meal.
Why include nuts and seeds in a pregnancy diet?
Nuts and seeds supply protein, healthy fats, vitamin E, and magnesium. Walnuts and chia seeds add omega‑3s for brain and eye development. A small handful makes a quick, nutrient‑dense snack.
Stir seeds into yogurt or sprinkle nuts over salads. I used a daily mix of pumpkin seeds and walnuts for steady energy and a bit of crunch.
Foods to Avoid During Pregnancy
Some foods raise the risk of infection or exposure to toxins. Knowing the short list makes decisions simple.
Why avoid raw or undercooked meats during pregnancy?
Raw or undercooked meat, seafood, and eggs can carry listeria, salmonella, or toxoplasma. These infections can lead to miscarriage, preterm birth, or severe newborn illness. Deli meats and hot dogs may carry listeria unless heated until steaming hot.
Skip raw sushi. Choose cooked options like vegetable rolls or cooked shrimp. The CDC reports that pregnant women are more likely to get listeriosis than others. Cooking meat fully is a reliable way to protect your baby’s growth.
What are the risks of unpasteurized dairy products?
Unpasteurized milk and soft cheeses like brie, Camembert, queso blanco, and blue‑veined varieties may contain listeria. Infection is uncommon but serious, with risks that include miscarriage or stillbirth. The CDC notes significantly higher risk in pregnancy.
Check labels and choose pasteurized milk, yogurt, and cheese. I craved soft cheese during pregnancy and switched to pasteurized options for safety.
Which fish are high in mercury and should be avoided?
Shark, swordfish, and marlin contain very high mercury levels and should be avoided. Mercury can harm a developing brain and nervous system. Limit oily fish to two portions weekly to stay within safe mercury limits while getting omega‑3s.
Canned light tuna has less mercury than albacore, but still eat it in moderation. Pick lower‑mercury fish most of the time to keep exposure down.
Why should alcohol and excess caffeine be limited?
Alcohol during pregnancy can damage a developing brain and organs at any stage. Health authorities advise no alcohol during pregnancy. Caffeine should be limited to about 200 mg daily, which equals roughly one 12‑ounce cup of coffee.
High intake may raise the risk of miscarriage or low birth weight. Ask your clinician about caffeine from coffee, tea, soda, energy drinks, and supplements.
How do added sugars and unhealthy fats affect pregnancy?
High amounts of added sugars and saturated fats increase extra calories and can lead to excess weight gain during pregnancy. This raises the risk of gestational diabetes and high blood pressure. Sugary foods also raise the chance of tooth decay.
Choose unsaturated fats from olive or canola oil and limit pastries, fried foods, and soda. Swapping a pastry for whole grain toast with nut butter helped me manage cravings and still meet nutrition goals.
Dietary and Caloric Recommendations
Calorie needs change across trimesters. Quality matters as much as quantity.
How should calorie intake change during each trimester?
First trimester: no extra calories needed. Focus on nutrient‑dense foods instead of “eating for two.” Second trimester: add about 340 calories per day. Third trimester: add about 450 calories per day.
Reach these targets with healthy snacks such as yogurt with fruit, a handful of nuts, or whole grain toast with eggs. Small meals spaced through the day can steady hunger and energy. This pattern also supports digestion and iron absorption.
Why eat smaller, frequent meals for better digestion?
Large meals can cause bloating or heartburn as the uterus presses on your stomach. Eating five or six smaller meals can reduce discomfort and keep blood sugar steady. A balanced breakfast often prevents midmorning cravings.
Many clinicians recommend this plan for easing nausea and constipation. I found that yogurt with fruit in the late morning kept me comfortable until lunch. Spreading iron‑rich foods across the day can also improve absorption.
Benefits of Hydration During Pregnancy
Think of fluids as the highway that moves oxygen and nutrients where they need to go.
Why is water important for amniotic fluid and circulation?
Water supports healthy amniotic fluid levels, which cushion your baby and allow movement. It also supports increased blood volume, which may rise by up to 50 percent to deliver oxygen and nutrients.
Many experts suggest at least 8 to 12 cups of fluids daily, more in heat or with exercise. I had fewer headaches and less swelling after increasing water during pregnancy.
What are healthy hydration alternatives like herbal teas and juices?
Plain water is best, but variety can help you meet your needs. Ginger or peppermint herbal teas are caffeine‑free and may ease nausea. Diluted 100 percent fruit juices, such as orange or apple, add vitamins like vitamin C.
Homemade vegetable soups also contribute fluids and minerals with less sodium. A small glass of cold orange juice gave me quick energy on busy mornings.
Safe Food Handling Practices
Food safety lowers the risk of illness for you and your baby. Simple habits make a big difference.
How to prevent foodborne illnesses like listeria and salmonella?
Keep raw meat and seafood separate from ready‑to‑eat foods like fruit, nuts, and salads. Use different cutting boards and knives for raw and cooked foods. Cook meat and poultry thoroughly, and avoid raw or runny eggs.
Wash produce under running water before eating. Keep your refrigerator at 40°F, 4°C, or lower. Pregnant women are at higher risk for severe illness from listeria and salmonella, so consistency matters.
What are proper washing and cooking techniques during pregnancy?
Rinse fruits and vegetables well. Scrub firm produce like potatoes and carrots with a clean brush. Heat ready meals until steaming hot, and reheat leftovers until piping hot throughout.
Cook eggs until yolks and whites are firm. Use a food thermometer for burgers, sausages, poultry, and whole cuts to confirm safe internal temperatures. During my pregnancy, I ate only fully cooked meats and hot leftovers to reduce food safety worries.
Role of Prenatal Supplements
Supplements do not replace food, but they help fill gaps. Your clinician can guide the best plan for you.
When and why should prenatal vitamins be taken?
Start a prenatal vitamin about three months before pregnancy if possible. Early folic acid intake lowers neural tube defect risk, which can form before many people know they are pregnant. Iron supports blood production and helps prevent anemia.
Choose a prenatal with at least 400 mcg folic acid and 27 mg iron. Continue throughout pregnancy to meet increased needs. Food first, plus a prenatal vitamin, offers reliable coverage.
How to consult with a healthcare provider about supplements?
Share your full medical history and all medicines, vitamins, and herbal products with your clinician. Some medicines, like certain anti‑seizure drugs, require higher folic acid. Ask which supplements are safe, which to avoid, and how to time doses with meals.
I brought a list of my vitamins to the first prenatal visit, which helped my doctor spot potential interactions. This simple step can protect both you and your baby’s development.
Healthy Snack Ideas for Pregnant Women
Snacks help you meet goals for protein, fiber, vitamins, and minerals without large portions.
What are nutrient-rich snacks suitable for pregnancy?
Try low‑fat yogurt with berries, hard‑boiled eggs, or apple slices with peanut butter. Whole grain crackers with cheese provide calcium and protein. Roasted chickpeas or mixed nuts add fiber and omega‑3s.
Crunchy vegetables like carrots and cherry tomatoes supply vitamins and help prevent constipation. A smoothie with leafy greens, banana, and fortified milk boosts folic acid and vitamin D. Use traffic light labels to compare packaged snack options quickly.
What are easy-to-prepare snack options for busy pregnant women?
Make small sandwiches or pita pockets with lean protein, salad greens, and a slice of cheese. Add a cup of low‑fat yogurt for extra calcium. Keep cans of bean soup on hand for fiber and iron.
Unsweetened cereal with milk is a fast choice. Pre‑pack sliced fruit, nuts, and seeds in resealable bags for grab‑and‑go options. In my third trimester, single‑serve bean salads with a sprinkle of chia seeds were perfect on busy days.
Special Dietary Considerations
Some health conditions call for extra planning. Work with your healthcare team for a plan that fits you.
How to manage diet for gestational diabetes?
Space meals evenly and pair carbs with protein to steady blood sugar. Choose high fiber foods like beans, lentils, vegetables, and whole grains. Limit added sugars and refined carbs, such as soda and white bread.
Include iron‑rich foods like eggs, spinach, or fortified cereals. Track portions and check glucose as directed. Water helps manage hunger without raising blood sugar. Planning snacks ahead helped me stay steady and meet growth goals.
What nutrition helps control high blood pressure during pregnancy?
Focus on foods rich in potassium, magnesium, and calcium. Bananas, oranges, leafy greens, beans, and low‑fat dairy support healthy blood pressure. Limit salty and processed foods.
Many studies link 1,000 mg of calcium daily with a lower risk of hypertensive disorders in pregnancy. Choose whole grains, add beans or lentils for fiber, and drink water instead of sugary drinks. Discuss changes with your clinician, especially if you take medication.
What should vegetarians and vegans consider during pregnancy?
Plant‑based eaters can meet needs with planning. Get protein from beans, lentils, tofu, nuts, seeds, and fortified cereals. Iron from plants absorbs better with vitamin C foods like citrus and tomatoes.
Vitamin B12 is found naturally in animal foods, so use fortified plant milks or a supplement. Choose calcium‑fortified soy or almond milk and include chia seeds, flaxseeds, hemp seeds, and walnuts for omega‑3s. Consider iodized salt or an iodine supplement if intake is low. A prenatal vitamin can help cover gaps, with guidance from your healthcare professional.
Conclusion
Eating a healthy diet supports you and your baby at every step. Key nutrients during pregnancy, such as folic acid, iron, calcium, vitamin D, protein, and omega‑3s, work together to power growth and protect your health.
Hydration, safe food handling, and smart choices about fish, caffeine, and alcohol reduce risks. Early planning and a quality prenatal vitamin improve confidence and outcomes.
For credible guidance, review resources from the CDC, ACOG, and the Dietary Guidelines for Americans. This article offers general education, not medical advice. Speak with your healthcare provider for personalized care and any questions about supplements or special diets.
FAQs
1. What are the most important nutrients for pregnant women?
Pregnant women need more protein, iron, calcium, folic acid, and vitamin D. These nutrients help support fetal growth and lower the risk of birth defects. For example, a 2020 study in The American Journal of Clinical Nutrition found that daily folic acid intake reduces neural tube defect risks by up to 70 percent.
2. How much weight should a woman gain during pregnancy?
Weight gain depends on pre-pregnancy body mass index (BMI). Most experts recommend gaining between 25 and 35 pounds if you start at a healthy BMI. Women with higher or lower BMIs may need different targets; your doctor can give specific advice based on your health needs.
3. Which foods should pregnant women avoid?
Pregnant women should not eat raw fish like sushi, unpasteurized dairy products such as some soft cheeses, deli meats unless heated until steaming hot, and high-mercury fish including shark or swordfish. These foods can carry bacteria or toxins that harm both mother and baby.
4. Can personal experience guide food choices during pregnancy?
Personal experiences often shape dietary habits but evidence-based guidelines provide safer direction for nutrition during pregnancy. For instance, I once craved soft cheese while expecting my first child but learned from my healthcare provider about listeria risks linked to unpasteurized cheese; this helped me make safer choices for myself and my baby.
Summary: Pregnant women benefit from eating nutrient-rich foods that supply key vitamins and minerals needed for healthy development. Following medical guidance helps ensure safe food choices throughout pregnancy while considering individual preferences within recommended limits.







