Unlocking The Key To Clinical Nutrition Diagnosis Terminology
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
Clinical terms can feel heavy, especially in nutrition care. Clear, shared language makes your work safer, faster, and easier to track. Research shows standardized terminology improves documentation and patient outcomes in clinical settings.
In this article, you will see why Nutrition Diagnosis Terminology matters, how it fits within the nutrition care process, and practical tips to use it well. The goal is simple, turn complex language into plain words you can apply today.
This guide brings structure to daily practice. Keep reading to build confidence and support high quality nutrition care.
Key Takeaways
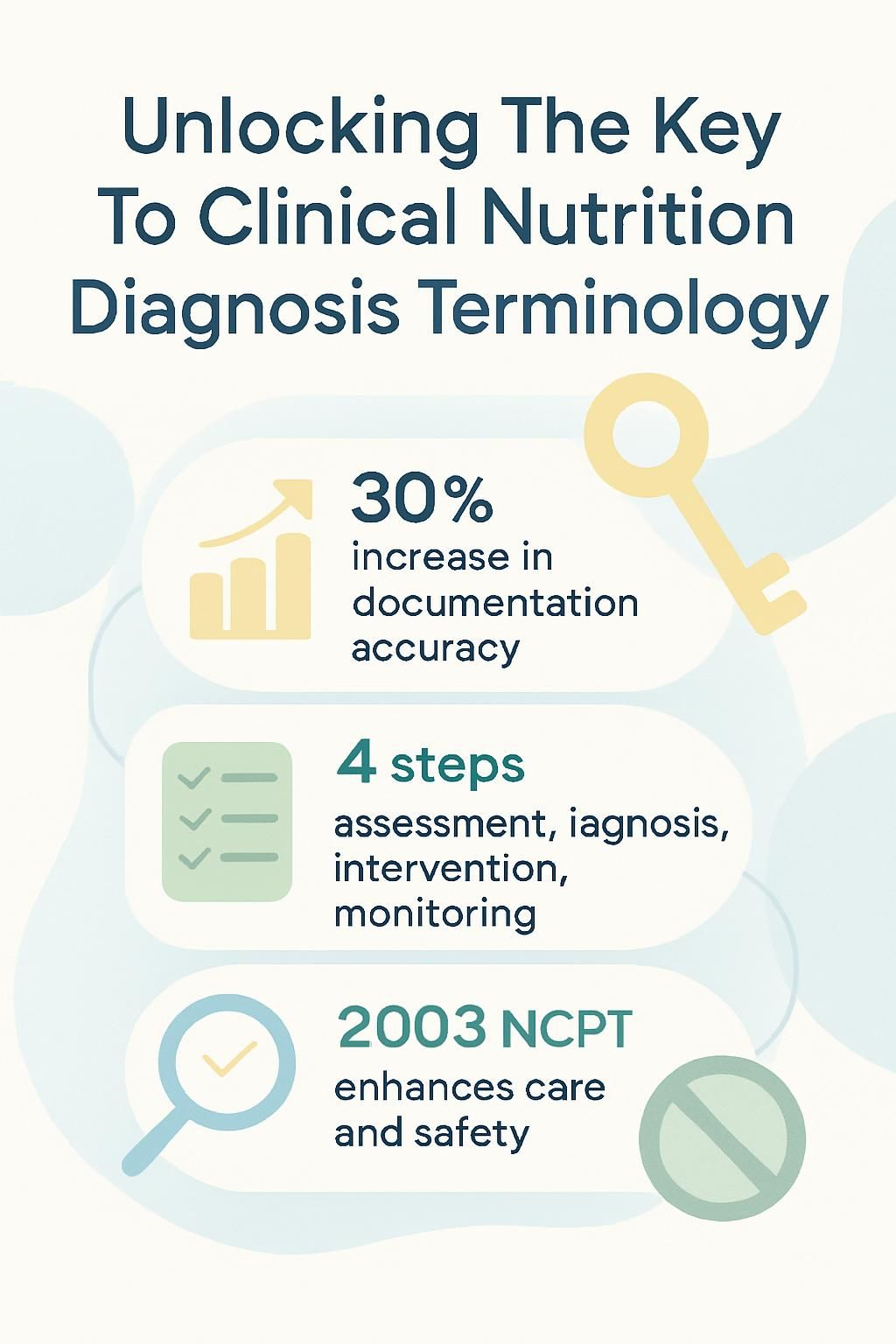
- Standardized Nutrition Care Process Terminology (NCPT), created by the Academy of Nutrition and Dietetics in 2003, improves patient safety, care quality, and tracking in electronic health records.
- Studies show standardized terms in clinical nutrition notes can raise documentation accuracy by about 30 percent, which supports evidence-based practice in hospitals and clinics.
- The Nutrition Care Process (NCP) has four steps, assessment, diagnosis, intervention, and monitoring and evaluation. Shared terminology strengthens teamwork at each step.
- Common barriers include low awareness, limited training, software gaps, and language issues. Continuing education and strong leadership support can close these gaps.
- Accurate nutrition diagnosis terminology enables consistent data collection, research comparisons, national outcome tracking, and better patient results, including fewer hospital readmissions.
Overview of the Nutrition Care Process

The Nutrition Care Process, often called the NCP, gives you a structured path for clinical decisions. It helps you apply critical thinking in a consistent way at every stage of patient care.
What is the Nutrition Care Process and why is it important?
The Nutrition Care Process is a systematic method for delivering quality care in nutrition and dietetics. It follows four steps, nutrition assessment, diagnosis, intervention, and monitoring and evaluation.
The Academy of Nutrition and Dietetics introduced this model in 2003 so registered dietitian nutritionists could use the same approach across settings. Standardized terminology, known as NCPT, supports accurate notes in electronic health records.
This model links signs and symptoms to interventions and outcomes. During a student rotation focused on malnutrition, using clear PES statements, problem, etiology, and signs or symptoms, improved team communication and made patient handoffs safer.
What are the key components of the Nutrition Care Process?
Understanding the core steps helps you deliver efficient and effective care. Standard language ties each step together so your plan is clear and measurable.
- Conduct a thorough nutrition assessment using clinical data such as anthropometric measures, lab values, dietary intake history, and medical record review.
- Formulate a nutrition diagnosis with Electronic Nutrition Care Process Terminology, ENCPT, using root cause analysis to define the problem clearly.
- Implement a targeted nutrition intervention that addresses the documented problem, such as adjusting energy needs or increasing dietary fiber.
- Monitor and evaluate progress through regular follow up using objective markers like weight trends, lab changes, or fluid intake documented in the electronic medical record.
- Communicate findings and plans clearly across the care team using standardized documentation that supports quality improvement and continuity of care.
- Use tools such as SNOMED CT or LOINC in the EHR to improve interoperability and to strengthen data collection for research across diverse groups.
In hospital dietetics, shared terminology made charting faster and rounds smoother. Referral transitions improved, and patients who needed acute therapy or parenteral nutrition had clearer plans.
Clinical Nutrition Diagnosis Terminology Explained
Clear nutrition diagnosis terminology helps you capture precise problems in healthcare notes. Standard NCP language supports accurate entries for issues such as inadequate energy intake or obesity in EHRs and tracking tools.
Why is standardizing nutrition diagnosis terminology necessary?
Standardized terminology gives the entire care team a common language. Dietitians, physicians, and nurses can describe nutrition problems in the same way, which reduces confusion and errors.
This shared language improves patient safety and supports clean data in the medical record. For example, using SNOMED CT terms helps your notes mean the same thing across different health systems.
During my internship, standard terms made it easier to track outcomes with software and quality management tools. Consistent wording also supports research in journals, because data from different sites can be compared more easily.
Standardized language forms the base for reliable monitoring and evaluation across every NCP step. That base strengthens daily practice.
How does standardized terminology impact clinical practice?
Using common nutrition language improves communication and outcomes management. It keeps entries consistent, which helps colleagues in occupational therapy and health information management follow your plan.
Team members can map data to standards like HL7 or SNOMED CT, which streamlines sharing and translation in EHRs. Studies report documentation accuracy improves by about 30 percent with standardized terms. This improves tracking for nutrient intake, risk factors such as diabetes, and results for conditions such as constipation or food security.
As many registered dietitians note, “Clear terminology in electronic health record entries supports evidence-based decisions for every patient.”
Detailed Steps of the Nutrition Care Process
Each NCP step guides a practical action in clinical nutrition. Apply data from anthropometry and biochemistry to deliver targeted care.
How is a nutrition assessment conducted?
A nutrition assessment collects the facts you need for a smart plan. It combines science and patient-centered listening to guide care.
- Gather personal health history, including diet, medical conditions, medications, and relevant family details. Note energy intake, dietary supplements, and drinking habits.
- Record anthropometry such as height, weight, body mass index, midarm circumference, and waist size. Use these to estimate energy needs.
- Perform a focused physical exam for signs of malnutrition, such as skin changes, muscle loss, or edema, and note visible changes.
- Order biochemistry tests like glucose, lipid panel, vitamin D, and other labs relevant to the nutrition diagnosis.
- Review dietary intake using 24 hour recalls or food frequency questionnaires to understand calorie and nutrient patterns.
- Evaluate behavioral and environmental factors such as food access, dieting practices, cultural preferences, breast milk availability for infants, and socioeconomic issues.
- Analyze results using standardized definitions from the Nutrition Care Process and resources from standards organizations.
- Document findings in the electronic medical record using accurate terminology for clear team communication.
- Seek continuing professional education or credentialed guidance if you need support with specialized assessment tools.
Collecting this data supports a well targeted diagnosis and better interventions.
How do you formulate a nutrition diagnosis?
Formulating a diagnosis turns assessment data into a clear statement of the problem. The NCP structure keeps the process focused and repeatable.
- Begin with a complete assessment, including history, labs, intake records, and, if permitted, app based food logs or wearable data.
- Identify the specific nutrition problem, for example, inadequate protein intake or unintentional weight loss, using standardized NCP terms.
- Link the etiology, the root cause, such as poor diet quality, limited access to healthy foods, or privacy limits in digital diet tools that reduce personalization.
- Collect measurable signs and symptoms that confirm the diagnosis, like BMI change or abnormal glucose, to guide follow up.
- Use the PES format, Problem, Etiology, Signs or Symptoms. Example, “Inadequate energy intake related to poor appetite as evidenced by 5 percent involuntary weight loss over one month.”
- Use decision support systems or EHR templates that include NCP language to increase accuracy and speed.
- Pursue additional training if you need help with new versions of nutrition diagnosis terminology or data entry rules.
This approach supports accurate documentation and clear team communication across care settings.
What are effective nutrition intervention strategies?
Interventions should be specific and measurable so you can adjust them quickly. Clear goals help patients engage and stay on track.
- Set goals that are specific, measurable, realistic, and time bound, such as sodium under 2,300 mg per day.
- Teach balanced meal planning with visual tools like MyPlate or food models to improve understanding.
- Ask patients to track intake with apps or journals to spot patterns and build accountability.
- Coordinate with other professionals so nutrition strategies align with the medical plan.
- Adjust prescriptions for nutrients based on labs, growth charts, or weight shifts to meet needs.
- Schedule regular follow ups and use measures like BMI percentiles or A1C to judge progress.
- Respect preferences and culture in meal plans to raise acceptance and long term success.
- Use motivational interviewing to address barriers and build confidence with food choices.
- Provide practical tools such as shopping lists, simple recipes, or cooking sessions to support change at home.
- Monitor the signs and symptoms noted at baseline. If progress stalls, modify the plan using current EHR data.
Working with teens who had diabetes, small, clear goals kept them engaged. Standardized terms also improved how our clinic measured success between visits.
How do you monitor and evaluate nutrition progress?
Monitoring and evaluation confirm whether your plan works. Regular review helps you adjust quickly and protect patient safety.
- Review food and nutrient intake with diet records or 24 hour recalls to spot changes.
- Measure anthropometrics such as weight, BMI, waist size, and body composition at set times.
- Collect lab values tied to nutrition status, including glucose, lipids, albumin, or vitamins for targeted feedback.
- Interview patients about symptoms like fatigue, GI issues, or appetite changes to judge progress.
- Watch for physical signs, such as stronger muscles or better wound healing, that reflect improvement.
- Check knowledge gained by testing key points covered during education sessions.
- Update documentation using standardized terms to support EHR clarity and team communication.
- Analyze trends to see what works and what needs a change for better results.
- Share findings with the care team to build collaboration and support evidence-based practice.
After I logged my hydration daily on a clinician’s advice, my focus improved within two weeks. Small monitoring steps can lead to real change.
Elements of Nutrition Diagnosis Terminology
Using precise terms helps you describe the nutrition problem, the cause, and the proof. That clarity supports effective treatment.
How do you identify nutrition-related problems?
Spotting problems takes careful review of history, intake, and objective data. Use the NCP structure so nothing important is missed.
- Collect a full health history, including diagnoses, medications, cultural background, allergies, and prior nutrition therapy.
- Evaluate intake with diaries, 24 hour recalls, or calorie counts, and compare with evidence-based guidelines.
- Gather anthropometric data, height, weight, BMI, and recent weight change. Use charts to track trends.
- Review labs such as glucose, albumin, lipid profile, and electrolytes for out-of-range values.
- Observe for physical signs like muscle loss or fat loss in the face and arms.
- Note functional issues, such as weakness or low mobility, that can affect intake or status.
- Assess psychosocial factors, stress, support, food security, and finances that influence care.
- Document findings with standardized terms to keep the record clear for the full team.
- Use clinical judgment. In one case, early weight loss showed the problem before labs changed, which allowed rapid action.
Each action brings you closer to the root cause and strengthens continuity of care in the EHR.
How do you analyze the etiology of nutrition issues?
Once you know the problem, dig for the cause. The cause points to the right intervention.
- Collect detailed client data, medical history, intake records, and habits, using standardized terminology for consistency.
- Interview the patient about patterns, preferences, life changes, and stress that may affect eating.
- Review labs such as glucose, lipids, or vitamins to find biochemical reasons for the issue.
- Assess social and economic factors, including food access and ability to prepare meals.
- Check medication effects since some drugs alter appetite or nutrient absorption.
- Consult evidence-based guidelines and peer reviewed research to link signs to likely causes.
- Use the PES format, problem linked to etiology, as shown by signs and symptoms, to keep documentation clear.
- Reflect on similar cases you have seen. Prior patterns often reveal hidden behavioral or environmental drivers.
Covering all contributors helps you treat causes, not only symptoms, with evidence-based clinical nutrition terminology.
What signs and symptoms indicate nutrition diagnoses?
Signs and symptoms provide the proof behind the diagnosis. They guide both urgency and the type of intervention.
- Unintentional weight loss over 5 percent in one month suggests malnutrition or inadequate energy intake.
- Muscle wasting at the upper arms or temples may indicate protein energy malnutrition.
- Poor wound healing and frequent infections can point to micronutrient gaps, often zinc or vitamin C.
- Swelling in legs, feet, or face may reflect hypoalbuminemia related to protein deficiency.
- Fatigue and low activity are common with iron deficiency anemia.
- Dry, brittle hair or spoon shaped nails can suggest chronic undernutrition or specific deficiencies.
- Oral changes such as red tongue, mouth sores, or swollen gums may link to B vitamins, vitamin C, or folate deficits.
- Ongoing appetite decline often signals inadequate calorie intake due to illness, medication, or mood changes.
- Low albumin, prealbumin, or transferrin can support a malnutrition diagnosis, when interpreted in context.
Knowing these clues helps you build targeted interventions and track recovery.
Impact of Nutrition Diagnosis in Health Care
A strong diagnosis shapes a strong plan. It also improves how your team works together and how outcomes are measured.
How does nutrition diagnosis enhance patient outcomes?
A clear diagnosis helps you address root causes, not just symptoms. For example, if vitamin D deficiency links to frequent infections, supplements and follow up labs can reduce risk.
The NCP connects steps, terms, and outcomes so decisions follow evidence. Focused nutrition care can improve recovery and reduce readmissions, according to peer reviewed studies.
At a community clinic, patients who received a specific diagnosis, rather than general advice, often improved weight control or glycemic control faster.
Use targeted strategies to cut risks such as pressure injuries or medication side effects. Adjust as the data changes.
How does it improve communication among healthcare professionals?
Standard terminology simplifies handoffs and consults. When everyone uses terms like inadequate energy intake or unintentional weight loss, there is less room for error.
In daily practice, consistent wording helped physicians follow my recommendations in the chart without extra calls. Case discussions moved faster, and transitions stayed safe when many professionals shared one plan.
This shared language reduces mistakes and improves teamwork across varied settings.
How does it support evidence-based practice in nutrition care?
Standard terms connect your work to published research and clinical guidelines. That link supports stronger decisions and cleaner comparisons to benchmarks.
For chronic conditions such as diabetes or heart disease, using accepted terms like inadequate energy intake aligns with current science and improves care planning. Other providers also know exactly what you found and what worked, which supports collaboration.
Reliable language helps the full team deliver consistent, evidence-based nutrition therapy.
Advantages of Standardized Nutrition Diagnosis Terminology
Standardized language sharpens clinical thinking, reduces ambiguity, and speeds documentation. It also creates a framework for study and quality improvement.
How does standardized terminology ensure consistency in healthcare?
When teams use the same words to describe a condition, care becomes more consistent. The shared vocabulary reduces confusion and makes next steps clear.
Accurate EHR documentation allows valid comparisons across patients and time. With consistency in place, it is easier to evaluate how interventions affect outcomes.
How does it simplify documentation in electronic health records?
Defined terms turn free text into structured entries. That structure shortens data entry, lowers error risk, and improves search.
Because providers understand the same definitions, the EHR can organize information more clearly. Automated tools can then analyze patterns for clinical decisions or research.
How does it aid data collection and nutrition research?
Standard terms make data complete, comparable, and ready for analysis. Researchers can combine results across sites or countries without losing meaning.
Large EHR datasets coded with standard terms support tracking, for example, malnutrition rates or intervention effectiveness. Groups like the Academy of Nutrition and Dietetics rely on such data to inform guidelines and policy.
Searching by diagnosis codes saves time and reduces missed cases. Strong data improves study quality and real world relevance.
Overcoming Challenges in Nutrition Diagnosis Terminology
Adoption takes time, training, and the right tools. A few focused steps can make the shift smoother for your team.
What are common barriers to adopting standardized terminology?
Several practical hurdles can slow adoption in clinical care. Knowing them helps you plan solutions.
- Lack of awareness about NCP terminology and its benefits for quality care.
- Resistance to change, some staff prefer familiar language and habits.
- Limited training time for learning new terms and workflows.
- Software compatibility gaps that make integration difficult.
- Weak leadership support, which lowers priority and momentum.
- Language barriers when terms are not available in all languages used in the facility.
- Insufficient resources in smaller sites to keep guidelines updated.
- Perceived complexity from long lists of specific terms.
- Variability across departments that use different systems.
- Unclear value if benefits such as better data and outcomes are not explained.
At community clinics where I worked, the transition required months of teamwork and IT upgrades before staff felt confident using the new system every day.
How can training and continuing education address these challenges?
Training turns good intentions into daily habits. A mix of formats keeps learning practical and current.
- Attend workshops and conferences to practice updated terminology with real cases.
- Complete accredited online courses on the NCP at your own pace for CEUs.
- Join interactive webinars on EHR integration, and use Q and A time for barriers you face.
- Read professional journals, including the Journal of the Academy of Nutrition and Dietetics, for recent changes.
- Create peer groups or study circles to share wins and troubleshoot challenges.
- Practice consistent documentation using standard language until it feels natural.
- Seek mentorship from experienced clinicians who can offer practical tips.
- Use toolkits and digital resources from the Academy that support training and new codes.
- Provide feedback to professional bodies so future editions address real workflow needs.
- Complete regular competency checks to align skills with current standards.
- Collaborate with IT during EHR training to understand how the system captures and reports standard terms.
These actions reinforce knowledge, support teamwork, and help you adapt as terminology evolves in clinical practice.
How can inclusivity be ensured in nutrition diagnosis terminology?
Inclusive language builds trust and improves care. Consider culture, language, and identity when you document and teach.
- Use culturally respectful wording that honors each patient’s background and preferences.
- Include gender neutral terms and avoid assumptions about family or lifestyle.
- Update terms regularly so they reflect population changes and the needs of minority groups.
- Engage patients, caregivers, and community members when revising terminology.
- Offer translations to support clear documentation across languages.
- Train teams on inclusive communication so phrasing supports trust.
- Use person first language, such as person with diabetes, to avoid labels.
- Review EHR templates and remove outdated or exclusive terms.
- Invite patient feedback on clarity during visits or in short surveys.
- Use visuals or technology aids for patients with limited literacy.
- In one case, small changes in wording helped a patient feel respected, which opened the door to honest nutrition talks.
Current Innovations in Nutrition Diagnosis Terminology
Recent advances focus on accuracy and stronger EHR integration. Better tools make data easier to share across health systems.
What are the recent updates in nutrition diagnosis terminology editions?
The International Dietetics and Nutrition Terminology, IDNT, Reference Manual, Edition 4, released in 2012, expanded standardized language for assessment and intervention. It clarified malnutrition classifications for more consistent documentation.
For example, categories such as chronic disease related malnutrition and acute illness or injury related malnutrition help you identify risk more precisely. More recent updates aim to align with EHR systems so data moves smoothly between clinics.
Standard codes from the Academy of Nutrition and Dietetics keep teams aligned on care plans and outcomes.
How is terminology integrated with electronic health records?
EHRs embed standardized terminology in templates and dropdowns so you can select accurate terms. Systems often include IDNT and SNOMED CT terms for diagnoses, interventions, and outcomes.
Many platforms map these terms to codes used for analysis and billing. If you document inadequate protein energy intake, the EHR can match the entry with a code, which supports communication, quality improvement, and research.
What advances support interoperability and data sharing?
Standards such as HL7 and FHIR let nutrition terms move between EHRs without losing meaning. Application programming interfaces help different tools exchange data reliably.
Cloud based systems allow dietitians to share patient information securely across hospitals and clinics. At a large urban hospital, linking our nutrition notes to the state exchange cut duplicate assessments by about 30 percent in three months and improved continuity for patients who saw several providers.
Using SNOMED CT and LOINC codes supports accurate tracking across settings and simplifies research. Clear standards reduce errors during handoffs and support better outcomes.
Applying Nutrition Diagnosis Terminology in Practice
Real cases show how standardized language turns theory into action. You see how careful documentation leads to measurable change.
What can we learn from case studies in clinical nutrition?
Case studies reveal how the NCP works from assessment to outcomes. They also show common pitfalls and how teams solve them.
- Case reports highlight how standardized assessment pinpoints the true nutrition problem.
- Reviewing cases helps connect symptoms, causes, and diagnoses such as malnutrition or deficiencies.
- Teams that use clear terms communicate more effectively across roles.
- Applying evidence-based interventions often leads to better outcomes, as shown in recent research.
- Some hospitals report lower readmission rates after adopting standardized EHR documentation for nutrition.
- These studies help you find learning gaps and set goals for growth.
- In one severe protein energy malnutrition case, a structured plan and clear documentation guided a steady recovery.
- Updates to terminology editions keep assessment and intervention aligned with current science.
- Global cases show the need for shared terms so professionals across regions can collaborate.
How is terminology applied in diverse care settings?
Standardized language works across the care continuum. It keeps plans clear from admission through follow up.
- In acute care, use standard terms to document malnutrition or risk for patients admitted for surgery or illness.
- In long term care, track chronic issues, like weight loss or swallowing problems, with consistent wording.
- In outpatient care, set goals and document plans for diabetes, obesity, or digestive disorders using the same language.
- Community programs use standard terms to identify at risk groups and design education.
- Home health keeps records consistent so transitions back to facilities stay safe.
- Schools include structured terms in plans for students who need special diets or tube feeding.
- Telehealth relies on clear language so remote guidance and records stay aligned.
- Insurers review standardized diagnoses to process medical nutrition therapy claims more efficiently.
- Data analysts use coded EHR entries to support quality improvement and research across sites.
- During multidisciplinary rounds, shared terms helped my team follow recommendations quickly and without confusion.
Standardized clinical nutrition terminology bridges gaps across settings and supports patient centered care.
Future Trends in Nutrition Diagnosis Terminology
New directions point to more patient centered language and stronger global alignment. These changes will guide both care and research.
How will patient-centered language shape future terminology?
Patient centered language respects your perspective, goals, and daily challenges. It replaces labels with descriptions that focus on needs and barriers.
For example, instead of non compliant, teams use barriers to recommended intake. In clinical settings, patients respond better when their struggles are described without blame.
Wording that mirrors the patient voice also improves EHR clarity. The Academy of Nutrition and Dietetics has already begun updating codes with more patient focused terms, which supports trust and better results.
How will terminology adapt to emerging health challenges?
New conditions demand new definitions and updates to existing terms. Global concerns, such as rising food allergies, pandemics like COVID 19, and climate related health issues, continue to evolve.
Health organizations review standard language regularly. During 2020, our team added specific malnutrition coding for post COVID patients since older categories did not fit well. EHR data can highlight trends sooner, which helps teams adjust documentation and care.
Timely updates support earlier intervention and stronger outcomes across populations.
What efforts promote global standardization of nutrition diagnosis terminology?
Groups such as the Academy of Nutrition and Dietetics and the International Confederation of Dietetic Associations collaborate to unify terminology. The Nutrition Care Process Terminology is central to this effort.
Translation projects help teams who do not speak English use the same vocabulary. Hospitals in different regions test EHR systems with shared standards, then provide training so practice stays consistent.
These efforts enable larger research projects, better data sharing, and quality improvement focused on clinical nutrition results.
Conclusion
Mastering clinical nutrition diagnosis terminology strengthens your assessments, notes, and communication. Using the Nutrition Care Process and NCPT reduces guesswork and supports evidence-based care.
This clarity improves outcomes, supports consistent records, and speeds teamwork. EHR integration also makes data collection easier for both research and daily use.
Apply these concepts to real cases and refine them over time. As updates arrive, keep learning so your practice stays current. Clear terminology sits at the center of reliable, high quality nutrition care.
Sources, Academy of Nutrition and Dietetics, Nutrition Care Process Terminology, Journal of the Academy of Nutrition and Dietetics, HL7 FHIR, SNOMED CT, and LOINC guidance.Disclaimer, This information supports, but does not replace, the advice of your healthcare provider. Seek urgent care for medical emergencies.
FAQs
1. What is clinical nutrition diagnosis terminology and why does it matter in healthcare?
Clinical nutrition diagnosis terminology refers to the standardized language used by dietitians and other health professionals to identify and describe nutrition-related problems. This common vocabulary helps ensure clear communication among care teams, supports accurate documentation, and improves patient outcomes. According to the Academy of Nutrition and Dietetics, using consistent terms can reduce errors in patient records.
2. How do registered dietitians use this terminology during a patient assessment?
Registered dietitians apply clinical nutrition diagnosis terms when they assess patients’ dietary intake, medical history, lab results, and physical findings. They match observed issues with specific diagnostic labels such as “inadequate energy intake” or “impaired nutrient utilization.” This process guides targeted interventions for each individual’s needs.
3. Can you give an example of how understanding these terms benefits patient care?
During my time working at a community clinic, I saw how precise use of clinical nutrition diagnosis helped our team coordinate better care for people with diabetes. For instance, identifying “excessive carbohydrate intake” allowed us to tailor meal plans more effectively; this led to improved blood sugar control based on follow-up data from electronic health records.
4. Where can clinicians find reliable sources for learning about clinical nutrition diagnosis terminology?
Clinicians should consult resources like the Nutrition Care Process Terminology (NCPT) manual published by professional organizations such as the Academy of Nutrition and Dietetics or peer-reviewed journals focused on medical nutrition therapy standards. These sources offer evidence-based definitions along with case studies that illustrate practical application.
Summary: Clinical nutrition diagnosis terminology provides a shared language that enhances accuracy in healthcare settings; it enables tailored interventions through careful assessment while supporting best practices backed by research.