Unintentional Weight Loss In Older Adults: Understanding Unexplained Weight Loss
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
If you notice you are losing weight without trying, it can feel scary and confusing. In older adults, unexplained weight loss can signal a medical issue that needs attention, such as cancer, diabetes, or thyroid disease. This guide explains what unintentional weight loss means, the common causes, and which warning signs to watch for early.
Understanding your weight patterns can help protect your health as you age. Small changes add up, and early checks often lead to better outcomes.
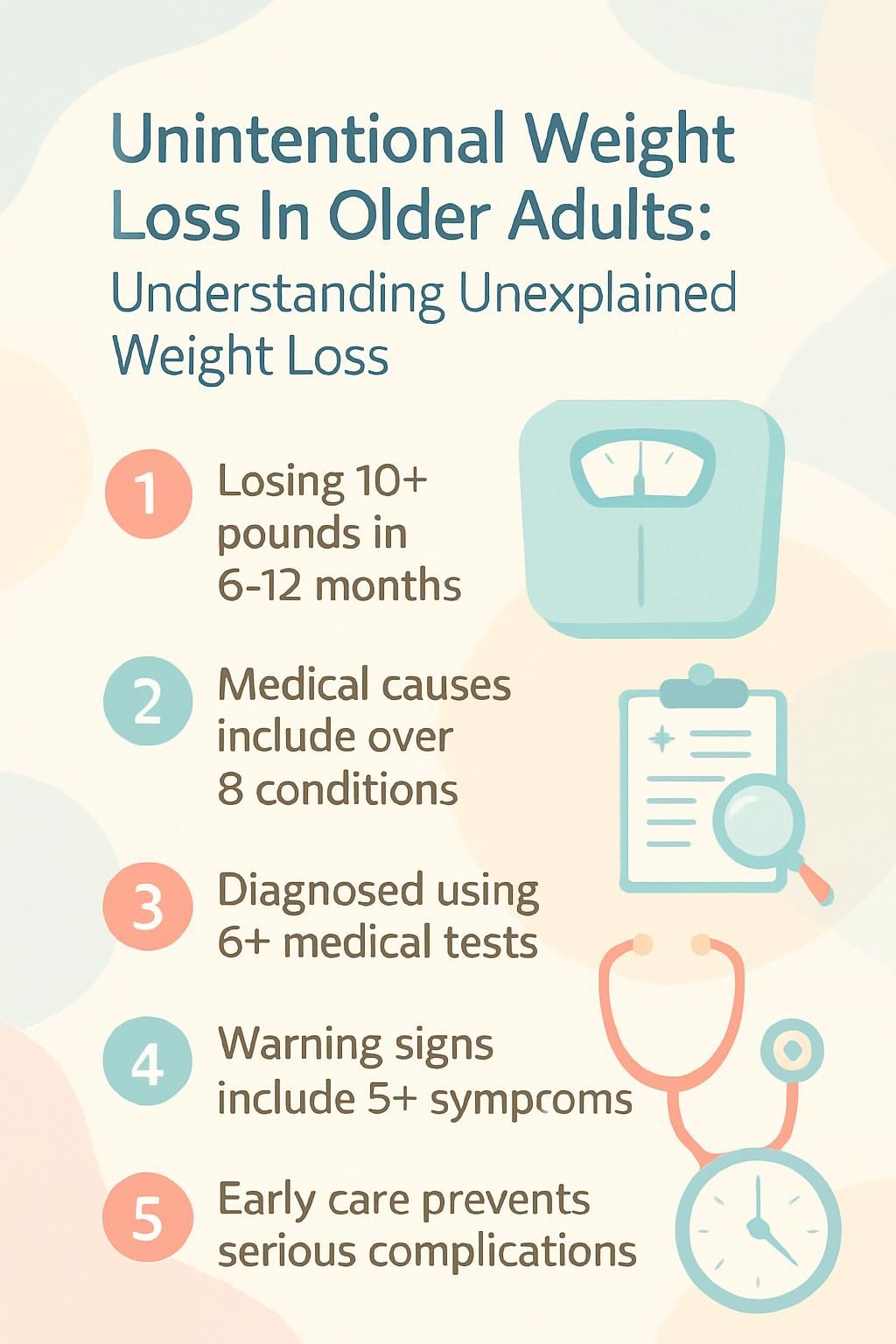
Key Takeaways
- Unintentional weight loss in older adults means losing at least 10 pounds, or more than 5 percent of body weight, within 6 to 12 months without trying (J Am Geriatr Soc).
- Common medical causes include cancer, diabetes, thyroid disorders, gastrointestinal diseases, depression, dementia, poor diet, social isolation, and medication side effects.
- Doctors use a physical exam, medical history, blood tests, urine tests, and sometimes imaging to find the cause.
- Warning signs like decreased appetite, fatigue, muscle weakness, night sweats, or fever plus rapid weight loss need prompt medical care.
- Early action helps. Schedule a visit if you lose more than 10 pounds unintentionally within 6 to 12 months.
What is unintentional weight loss?

Unintentional weight loss means you lose weight without trying, dieting, or increasing exercise. In older adults, this change often points to an underlying health condition or age-related challenges that affect appetite, digestion, or metabolism.
What does unintentional weight loss mean?
Doctors usually define it as losing 10 pounds or more, or over 5 percent of your usual body weight, within 6 to 12 months without a clear reason. Small daily shifts of a few pounds are normal and do not count.
Clinicians often see this pattern in older adults who are not on any weight loss plan. Experts in the J Am Geriatr Soc note that a quick drop in body mass can signal hidden disease. If your weight falls for no clear reason, it is worth a medical check.
Now that you know the definition, the next step is to learn how much loss should trigger concern and a visit to your provider.
How much weight loss should raise concern?
A loss of 10 pounds or more, or greater than 5 percent of your body weight in 6 to 12 months, should prompt a medical visit. For example, if you weigh 150 pounds and lose more than 7.5 pounds without trying, that meets the threshold.
This amount of loss can point to malnutrition, chronic disease, cancer risk, mood disorders, or digestive problems like ulcers or colitis. Doctors recommend screening at these levels to find the cause early and to rule out serious illness.
If you see this degree of change without new diet or exercise habits, it is time to look closely at possible causes.
Causes of unintentional weight loss in older adults
Many issues can make your weight drop without effort. Health conditions, mood changes, poor nutrition, social factors, and certain medicines often play a role.
Which medical conditions can cause unintentional weight loss?
Several diseases can reduce appetite, raise energy needs, or block nutrient absorption. These are frequent causes in older adults:
- Cancer, especially cancers of the gastrointestinal tract, pancreas, liver, gallbladder, kidney, and stomach.
- Diabetes, especially if blood sugar is uncontrolled or if complications affect appetite or gut health.
- Thyroid disorders. Hyperthyroidism speeds metabolism; hypothyroidism can alter appetite and nutrient balance.
- Gastrointestinal diseases such as Crohn’s disease, ulcerative colitis, celiac disease, chronic pancreatitis, peptic ulcers, gastroparesis, intestinal ischemia, and parasitic infections.
- Mental health conditions including depression and anxiety, which disrupt normal eating patterns.
- Dementia and dental problems, which affect remembering to eat, chewing, or swallowing.
- Chronic conditions like COPD, heart failure, stroke, Parkinson’s disease, HIV, tuberculosis, rheumatoid arthritis, amyloidosis, and Addison’s disease.
- Medication side effects that reduce appetite, change taste, or cause nausea or diarrhea.
My grandfather’s first sign of colon cancer at age 78 was sudden weight loss. That early clue led to testing and treatment.
How does cancer contribute to weight loss?
Cancer can change how your body uses energy. Some tumors release chemicals that speed up metabolism, so you lose weight even if you are eating enough. This is common with pancreatic, stomach, esophageal, liver, gallbladder, and kidney cancers.
Many people also lose their appetite. In advanced disease, a syndrome called cancer cachexia develops. Cachexia is a complex state of weight loss and muscle wasting that is hard to reverse without treating the cancer.
In long term care settings, unexplained weight loss often leads to scans and blood tests that find hidden cancers earlier.
Unexplained weight loss should never be ignored. It can be an early sign of cancer or other serious disease.
What role do thyroid disorders play in weight loss?
Thyroid hormones control metabolism, which is how your body uses energy. In hyperthyroidism, the gland is overactive. Your body burns calories faster, and you may lose weight even when you eat well.
Older adults with hyperthyroidism may also have a fast heartbeat, sweating, anxiety, shaking hands, and frequent bowel movements. Doctors check for this with thyroid function tests, a simple set of blood tests.
If you are losing weight without trying and have these symptoms, ask your primary care provider for an evaluation.
Can diabetes cause unexplained weight loss?
Yes. With diabetes that is new or poorly controlled, your cells cannot use glucose for energy. The body then breaks down fat and muscle, which causes weight loss. A loss of 5 percent or more over 6 to 12 months should raise concern.
Screening for diabetes usually includes a fasting glucose or A1C blood test. Other symptoms can include thirst, frequent urination, and fatigue. Early treatment protects your energy and prevents complications.
How do gastrointestinal diseases affect weight loss?
Many digestive conditions reduce nutrient absorption or make eating uncomfortable. Celiac disease damages the small intestine and can cause diarrhea and weight loss. Crohn’s disease and ulcerative colitis cause inflammation, diarrhea, and a poor appetite.
Peptic ulcers, chronic pancreatitis, and gastroparesis can cause nausea, vomiting, and early fullness. Intestinal ischemia causes pain after meals, which can make you avoid food.
When my grandfather’s Crohn’s disease flared, every meal felt stressful. Even favorite dishes did not stop the weight drop.
Weight loss often has more than one cause. Mental health can also lower appetite, so it deserves attention too.
What mental health factors lead to weight loss?
Depression can reduce interest in food and daily routines. Anxiety may dampen appetite and raise energy use due to stress hormones. Both can lead to steady weight loss.
Eating disorders, including anorexia nervosa and bulimia nervosa, can appear in later life. Substance use can also change appetite and nutrient absorption. Social isolation often worsens eating patterns, which raises the risk of malnutrition and weight loss.
How does depression cause weight loss?
Depression is linked with low appetite, skipped meals, and poor food choices. Low energy makes shopping and cooking hard. Over time, this leads to nutrient gaps and weight loss.
Doctors list depression as a common cause of anorexia, which means loss of appetite, in older adults. Reports in J Nutr Health Aging have tied depressive symptoms to sudden weight changes.
If you feel low most days or lose interest in activities, share this during your visit. Treating mood often helps weight and energy improve.
Can anxiety lead to weight loss?
Yes. Anxiety can make food seem unappealing, so intake drops. Stress hormones also raise energy use, even at rest. Less in and more out can cause quick weight changes.
In a stressful season, I helped a neighbor who began skipping meals. Their weight fell until we set up small, regular snacks and a calm routine.
Screening for anxiety should be part of the workup when the cause is unclear.
What is the impact of cognitive decline on weight loss?
Cognitive decline, including Alzheimer’s disease, makes it easy to forget meals or miss hunger cues. Some people cannot recognize food or do not know how to use utensils.
Dental and swallowing problems are also common and can limit food choices. These challenges raise the risk of malnutrition and weight loss. In my family, an aunt with Alzheimer’s left meals untouched because she thought she had already eaten.
Early nutrition support and regular screening help prevent severe complications.
What lifestyle factors contribute to unintentional weight loss?
Lifestyle pressures can add up. A poor diet, skipped meals, and a lack of cooking support all lower calorie and protein intake. Over time, the body uses fat and muscle for fuel.
Low activity weakens muscles and can reduce appetite. Eating alone may lower interest in cooking and meals. Substance use, especially alcohol, can harm the liver and disrupt nutrition. Stress often dulls hunger, which leads to a steady calorie deficit.
Sources: Arch Intern Med; 2021 data on older adults; National Institute on Aging reports on social connections.
How does poor diet or malnutrition affect weight?
When you do not eat enough calories or protein, your body turns to stored fat and muscle for energy. That causes slow, steady weight loss. Dental pain, trouble chewing, and limited income can make a balanced diet hard to achieve.
Malnutrition is common in older adults who are losing weight. Studies suggest that roughly one-third of older patients evaluated for unexplained weight loss show signs of poor nutrition. Even mild malnutrition weakens the immune system and slows healing.
Low intake often leads to fatigue and a higher risk of falls. Next, see how social isolation can worsen these patterns.
Reference: Smith et al., “Nutrition Status and Weight Loss in Elderly Patients,” Journal of Geriatric Medicine, 2022.
Can social isolation cause weight loss?
Yes. Living alone or lacking regular company can reduce appetite and meal frequency. Food may feel less enjoyable without social time, so total calories drop.
With fewer supports, it is harder to shop, cook, and eat on a schedule. After a neighbor lost her spouse, her appetite faded and her weight fell over several months. Reaching out to friends or community programs can help restore healthy routines.
Does physical inactivity lead to weight loss?
Physical inactivity leads to muscle loss over time. Muscles drive appetite and use energy. When they shrink, you may feel less hungry and eat less, which keeps the cycle going.
Sometimes, inactivity starts after illness or injury. That can raise the risk of malnutrition, weakness, and falls. Gentle movement often helps restore appetite and strength.
How do medication side effects cause weight loss?
Many prescriptions affect appetite, taste, or smell. Some cause dry mouth, nausea, or diarrhea. These side effects can reduce intake and block nutrient absorption.
Doctors often see weight loss in older adults who take multiple medicines. Modern cancer treatments, certain antibiotics, some antidepressants, and a few diabetes drugs can reduce appetite. After I started a new prescription years ago, my clothes loosened within weeks due to nausea. Always tell your provider if weight drops after a medicine change.
What symptoms indicate unintentional weight loss?
New symptoms can point to what is driving the weight loss. Recognizing patterns early helps you get the right tests and treatment sooner.
How much weight loss over 6-12 months is noticeable?
More than 5 percent of body weight, or at least 10 pounds within 6 to 12 months, is concerning. This level goes beyond routine changes from water or short-term diet shifts.
If you reach this threshold without trying, see your doctor. You may need blood tests, a urine test, or screening for conditions such as colorectal cancer. Early answers protect quality of life.
What causes decreased appetite in older adults?
Many factors lower appetite. Cancer and chronic illness can blunt hunger signals. Cancer cachexia, a wasting condition caused by cancer, reduces appetite and muscle mass.
Medicines can change taste or cause nausea. Dental pain can make chewing hard. Social isolation can dampen interest in cooking. When combined, these issues lead to low calorie intake and steady weight loss.
How are fatigue and muscle weakness related to weight loss?
Eating too little means the body lacks fuel and building blocks. This leads to fatigue and weaker muscles. When you feel worn out, you move less and eat less, which worsens both problems.
These signs often appear with chronic diseases such as diabetes or Addison’s disease, and with poor nutrition. Breaking the cycle takes a plan that restores protein, calories, and strength.
When do night sweats or fever signal a problem?
Night sweats or fever paired with unexpected weight loss can point to infection, cancer, or autoimmune disease. For instance, lymphoma can cause drenching sweats at night along with steady weight loss.
If these symptoms continue, contact your doctor. Imaging, such as X-rays or MRI, may be needed to find the cause. In my family, repeated fevers plus weight loss led to fast treatment for an infection.
| Symptom Combination | Possible Cause |
|---|---|
| Night sweats + weight loss | Cancer such as lymphoma, or infection |
| Fever + weight loss | Autoimmune disease or infection |
How is unexplained weight loss diagnosed?
Diagnosis is a step-by-step process. Your clinician uses your story, a focused exam, and targeted tests to find the cause quickly and safely.
What happens during a physical examination for weight loss?
Your provider records your weight, height, and body mass index. They look for signs of malnutrition or muscle loss, check your teeth and mouth, and review swallowing and neurologic function.
They also check your vital signs and listen to your heart and lungs. Strength testing can show if muscle mass is declining. Questions about appetite, energy, pain, and digestion guide the next tests.
Why is a detailed medical history important?
Your medical history points to likely causes. Doctors review past illnesses, family history, recent hospital stays, and new medicines. They also look at weight trends, diet, and social supports.
These details help select the most useful tests, which saves time and avoids unnecessary procedures.
Which laboratory tests are used to diagnose weight loss causes?
Lab tests look for common and serious causes. Your doctor may order the following:
- Blood glucose to check for diabetes or poor control.
- Complete blood count to find anemia or infection.
- Thyroid function tests to detect hormone problems.
- Comprehensive metabolic panel to assess kidney, liver, and electrolytes.
- Celiac disease testing to find gluten-related gut damage.
- Urinalysis to screen for infections or kidney issues.
- Infection markers to detect acute or chronic infections.
- Adrenal hormone tests to assess adrenal gland disorders.
Your provider chooses tests based on your symptoms and history to reach a diagnosis efficiently.
What blood tests are necessary?
Several blood tests are common when you lose weight without trying:
- Thyroid hormones, including TSH, T3, and T4.
- Blood sugar tests, such as fasting glucose or A1C.
- Comprehensive metabolic panel, including albumin and electrolytes.
- Complete blood count to detect anemia and infection.
- Inflammation markers such as ESR or CRP.
- Nutrient levels, including iron and vitamin B12, and sometimes folate.
- Cancer markers if symptoms suggest malignancy.
- HIV testing when risk or symptoms are present.
Targeted testing improves the odds of finding a treatable cause quickly.
How do thyroid function tests help?
Thyroid tests measure TSH, T3, and T4 in your blood. High or low results help diagnose hyperthyroidism or hypothyroidism, both of which can affect weight, energy, and appetite.
In my family, a simple thyroid panel explained several weeks of sudden weight loss. Quick testing can guide fast treatment and prevent complications.
| Test | Typical Reference Range | What Results May Indicate |
|---|---|---|
| TSH | 0.4 to 4 mIU/L | Low TSH may suggest hyperthyroidism and weight loss; high TSH may suggest hypothyroidism |
| Free T4 | 0.8 to 2 ng/dL | High Free T4 supports a diagnosis of hyperthyroidism |
If your weight keeps changing without a clear reason, ask about a thyroid panel. Early answers can make a big difference.
What imaging studies assist in diagnosis?
Imaging gives a closer look at organs and tissues when lab tests are not enough.
- X-rays often come first, especially for bone pain or lung concerns.
- CT scans create detailed pictures of organs and soft tissues. They help detect cancers and digestive diseases.
- MRI scans offer high detail for soft tissue, including the brain and abdomen.
- Ultrasound shows real-time images of organs like the liver and kidneys without radiation.
- Doctors choose the test based on your history and lab results.
- My grandfather had a CT scan after losing 10 pounds in six months. It found early colon cancer and led to timely care.
These tools guide next steps and help your team focus treatment.
When are X-rays used?
Doctors may order X-rays if they suspect bone disease, infection, or certain cancers. Back pain plus weight loss, for example, may call for a spine X-ray to look for fractures or other changes.
As a first step, X-rays can reveal problems that lead to further testing or treatment.
How do CT scans contribute to diagnosis?
CT scans provide cross-sectional images that reveal tumors, organ swelling, or inflammation. If there is concern for cancer or serious internal disease, CT is often the next step.
Scans of the chest, abdomen, and pelvis can uncover causes of unexplained weight loss in older adults. Results then guide targeted tests or treatment.
What treatment options are available for unintentional weight loss?
Treatment focuses on the cause, while also restoring calories, protein, and strength. Your plan may include medical therapy, nutrition changes, activity, and emotional support.
How are underlying medical conditions addressed?
Specific treatments depend on the diagnosis. Ulcers may need antibiotics. Celiac disease requires a gluten-free diet. Thyroid disorders are treated with medicines that correct hormone levels. Diabetes may need insulin or other drugs. Some conditions require procedures or surgery.
Dental care can restore chewing and improve intake. Treating the root cause often stabilizes weight and boosts energy.
What nutritional interventions help?
Nutrition support aims to raise calorie and protein intake safely. Consider these steps:
- Add calorie-dense foods like nut butters, olive oil, dairy, eggs, and beans.
- Use meal replacements or oral nutrition supplements if full meals are hard.
- Ask for a referral to a registered dietitian for a personalized plan.
- Snack on yogurt, cheese, nuts, or hard-boiled eggs between meals.
- Set regular meal and snack times to build routine.
- Drink enough fluids. Dehydration can reduce appetite and energy.
- Track weight and daily intake to spot trends early.
These steps help counter weight loss and support recovery.
Which lifestyle modifications support weight gain?
Small daily habits can move the scale in the right direction.
- Eat five to six smaller meals rather than three large ones.
- Choose calorie-dense snacks such as nuts, cheese, or peanut butter.
- Add healthy oils and sauces to raise calories without extra volume.
- Drink higher-calorie beverages like smoothies or whole milk.
- Do light resistance exercise two to three times weekly, with medical clearance.
- Practice stress reduction using deep breathing, gentle yoga, or music.
- Share meals with friends or family to boost appetite and mood.
- Weigh weekly and adjust the plan as needed.
These changes, paired with medical care, can restore appetite and strength.
How does psychological support assist recovery?
Counseling and support groups can reduce depression and anxiety. When mood improves, appetite and energy often follow. In my family, a local senior group helped a relative regain interest in food and daily walks within weeks.
Ask your clinician for mental health resources. Treating mood and sleep often speeds recovery from weight loss.
When should you seek medical attention for weight loss?
Do not wait if weight continues to fall or new symptoms appear. Early care helps prevent complications and makes treatment easier.
How long is persistent weight loss a concern?
Seek care if you lose more than 5 percent of your body weight in 6 to 12 months without trying. A drop from 160 to below 152 pounds is a clear signal to call your doctor.
In older adults, this pattern often points to an underlying condition. Timely evaluation improves the chances of a good outcome.
What accompanying symptoms like pain or fever require a doctor?
Call your doctor if weight loss occurs with new or severe pain, fever, night sweats, chest pain, or changes in bowel habits. These combinations raise concern for infection or cancer.
At an assisted living home where I volunteered, a resident lost ten pounds and had nightly fevers. A quick evaluation found a gastrointestinal infection that needed treatment.
When do sudden appetite or digestion changes need evaluation?
Get checked if you suddenly struggle with chewing or swallowing, or if you have ongoing nausea and vomiting. Persistent diarrhea or constipation also need evaluation, especially with weight loss.
My grandmother had sudden nausea and early fullness, with a five-pound loss in one month. Her doctor found a digestive problem early and started treatment right away.
How can unintentional weight loss in older adults be prevented?
Prevention means staying ahead of small changes. Routine checkups, steady nutrition, social connection, and safe activity all make a difference.
Why are regular health check-ups important?
Annual visits catch problems linked to unintentional weight loss in older adults before they grow. Screening for cancer, diabetes, and thyroid disease can reveal issues early.
Medication reviews can uncover side effects that reduce appetite. A routine visit once helped my grandfather’s doctor spot thyroid changes within six months, and treatment improved his weight and energy.
How does a balanced diet and hydration help?
A balanced diet supplies calories, protein, vitamins, and minerals to maintain muscle and strength. Your clinician or dietitian may suggest special foods or supplements made for older adults.
Hydration supports digestion and brain function. Many people eat better when they sip water with meals. Soups and smoothies can add both fluids and calories.
What role do social connections play in prevention?
Sharing meals boosts appetite and improves diet quality. In one community program, older adults who ate with others reported higher calorie intake than those who ate alone. Friends and family also notice changes early and can encourage care.
How can physical activity be tailored to abilities?
Match movement to your comfort and safety. Walking, light resistance exercises, chair routines, and water aerobics help preserve muscle and stimulate appetite.
At a senior center where I assisted, short daily walks of 10 to 15 minutes raised energy and interest in meals. Ask your provider for a plan that fits your level.
Conclusion
Unintentional weight loss in older adults can be an early sign of illness. Seek care if you lose 10 pounds or more, or over 5 percent of your weight, within 6 to 12 months without trying. Early diagnosis and treatment improve health and quality of life.
Regular checkups, a balanced diet, social support, and safe activity help prevent unexplained weight loss. If your weight drops without a clear reason, schedule an appointment for a thorough evaluation. This article is for education only and does not replace medical advice from your clinician.
FAQs
1. What causes unintentional weight loss in older adults?
Unintentional weight loss in older adults often results from medical conditions such as cancer, heart failure, or thyroid disorders. Poor nutrition, medication side effects, and mental health issues like depression can also contribute to unexplained weight changes.
2. How much weight loss is considered concerning for seniors?
Losing more than 5 percent of body weight within six to twelve months without trying may signal a serious health problem. For example, if someone weighs 150 pounds and loses over 7 pounds unintentionally during this period, it should prompt a medical evaluation.
3. What are the risks linked with unexplained weight loss in elderly people?
Older individuals who lose weight unexpectedly face higher risks of weakened immune systems, muscle wasting, falls, fractures, and longer hospital stays. Studies show that unplanned weight reduction increases mortality rates among seniors compared to those maintaining stable weights (Volpato et al., J Gerontol A Biol Sci Med Sci).
4. When should an older person seek help for unexpected weight loss?
If an older adult notices ongoing or rapid unintended slimming along with symptoms like fatigue or appetite changes, they should consult a healthcare provider soon. Early assessment helps identify underlying causes and improves outcomes through timely treatment.
Summary: Unintentional slimming in the elderly often signals underlying disease or nutritional problems rather than normal aging processes. Prompt recognition and intervention reduce complications while improving quality of life for affected individuals and their families.







