Unlocking Nutritional Insights: The Power Of Nutrition Assessment
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
Low energy, sudden weight changes, or frequent illness can signal gaps in your diet. A nutrition assessment turns your food choices and health data into clear next steps. It helps you spot problems early and choose a plan that fits your life.
This guide explains why a thorough nutrition assessment matters, the steps involved, and how key numbers tie to issues like malnutrition or obesity. You will also see practical tools you can start using today.
Key Takeaways
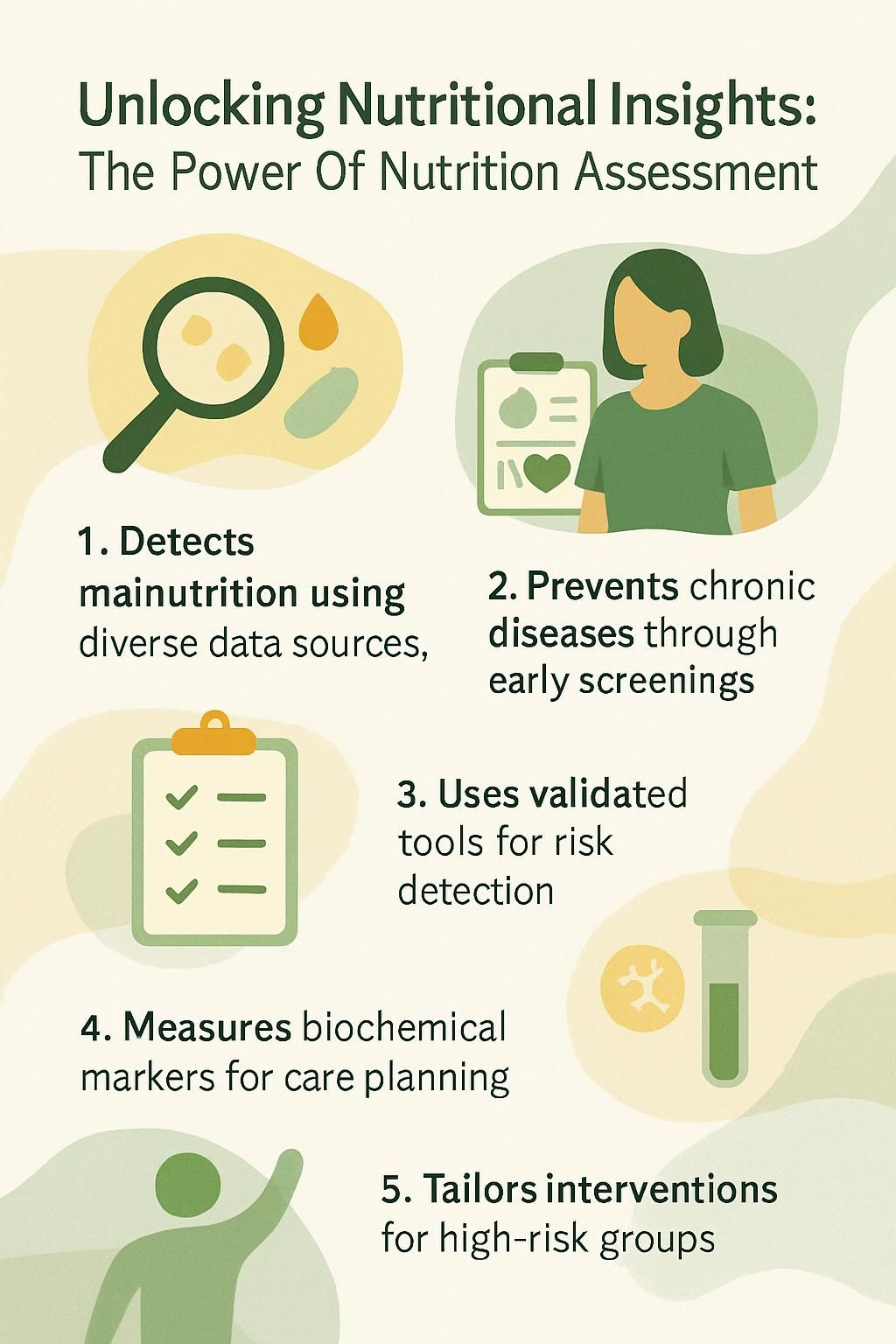
- Nutrition assessment combines dietary reports, lab tests, body measurements, and medical history to find nutrient gaps early. Leading groups such as the Academy of Nutrition and Dietetics recommend routine screening.
- Regular screening helps prevent complications from chronic conditions like diabetes and heart disease. Evidence shows better outcomes, shorter hospital stays, and lower costs (Thomas et al., 2016).
- Validated tools, including the Mini Nutritional Assessment for older adults and Food Frequency Questionnaires, improve detection of nutritional risk in many populations.
- Common biochemical tests include albumin, prealbumin, iron studies, vitamin B12, C-reactive protein, glucose, and lipids. These results guide care plans.
- Registered dietitians work in teams to tailor care for high risk groups, such as pregnant women and older adults, using Dietary Reference Intakes from the US Food and Nutrition Board.
Understanding Nutrition Assessment

Nutrition assessment gives you a clear picture of how your eating patterns affect your health. It can reveal risks early, so you can act before small issues grow.
What is Nutrition Assessment and What Are Its Goals?
Nutrition assessment evaluates your nutritional status, which means your body’s supply of nutrients. It reviews dietary intake, medical history, a physical exam, anthropometric data such as height, weight, and body mass index, and biochemical data from lab tests.
The goals are simple and practical:
- Find people who face a high risk of malnutrition or deficiency.
- Identify causes such as poor appetite, illness, or limited access to food.
- Create a personalized plan, then monitor change over time.
- Measure what works and adjust the plan when needed.
Screening tools like the Mini Nutritional Assessment help flag risk in older adults. Dietary Reference Intakes offer safe targets for nutrient needs across ages. Working with a dietitian, you can use these tools to meet your goals and improve outcomes.
What Are the Essential Elements of a Nutrition Assessment?
A complete assessment uses several connected parts. Each one adds a piece to the picture.
- Dietary Assessment reviews foods and beverages consumed, meal patterns, cooking methods, portion size, and recent changes. Tools include the 24-hour dietary recall and Food Frequency Questionnaires.
- Anthropometric Measurements track height, weight, BMI, waist size, and body composition. These numbers show weight trends that signal risk.
- Biochemical Tests analyze blood and urine for proteins, vitamins such as vitamin B12, electrolytes, and glucose. A complete blood count helps spot anemia and infection.
- Medical History Evaluation covers diagnoses, medicines, surgeries, digestive symptoms, and family history of conditions like type 2 diabetes.
- Nutrition-Focused Physical Findings look for muscle loss, loss of under-skin fat, mouth ulcers, and skin changes linked to deficiencies. Functional checks such as strength for daily tasks show how nutrition affects life.
- Socioeconomic and Lifestyle Factors include access to healthy foods, nutrition knowledge, cultural practices, sleep, stress, and activity level.
- Team-Based Coordination brings dietitians, doctors, nurses, and therapists together. Shared data improves accuracy and supports better care planning.
In a large hospital, this complete approach helped patients with diabetes and cancer-related weight loss regain strength faster. The lesson is clear, detailed data leads to better plans.
The Significance of Nutrition Assessments
Good assessment acts like an early-warning system. It points to nutritional risk before it becomes a crisis.
How Can Nutrition Assessments Detect Nutritional Risks and Deficiencies?
Screening tools look for red flags such as major weight loss. Losing more than 10 percent of usual weight within months signals high risk. Dietitians also watch for hair loss, slow wound healing, swelling, or bleeding gums. These can point to vitamin or mineral shortages.
Anthropometry, the sizing and measuring of the body, tracks changes in muscle and fat. Lab tests catch problems with electrolytes, protein levels, and red blood cells. Medical diagnoses like type 2 diabetes raise risk over time and deserve close follow-up.
Unplanned, rapid weight loss is a strong warning sign of malnutrition risk.
Screening also sorts risks using common categories, such as undernutrition, micronutrient shortages, overnutrition, and diet-related diseases.
How Do Nutrition Assessments Promote Health and Well-being?
Early assessment lets you act while problems are still small. Fixing low protein stores or fast body changes can improve healing and lower infection risk. In hospitals, this can shorten recovery time and reduce complications.
High risk groups such as infants, children, pregnant women, and older adults benefit most. Early help prevents long term issues like stunted growth or severe weight loss. Better nutrition also supports immunity, energy, and mood.
How Are Personal Care and Interventions Tailored Using Nutrition Assessments?
Results guide a plan that fits your needs. Dietitians use your food history, body composition, lab data, and physical signs to find the root cause of the problem. Then they set a plan you can follow.
Example, low iron stores plus heavy periods and fatigue call for higher iron intake, food sources first, then supplements if needed. Follow-up checks show what is working. Your plan evolves as your lab values and daily life change, following standards from the Academy of Nutrition and Dietetics.
Key Components of a Nutrition Assessment
Each component offers a different lens on your nutritional status. Together, they support clear decisions and better monitoring.
How Is Dietary History Examined in Nutrition Assessment?
Dietary history is collected using interviews and standardized tools. The 24-hour recall, Food Frequency Questionnaires, and food tracking apps are common. You note meals, snacks, portion size, cooking methods, and any diet rules or allergies.
Special diets need extra care. For example, a vegan diet can lack vitamin B12 without careful planning. Clinicians also review supplements, enteral and parenteral nutrition, and any feeding issues that could limit intake.
What Are Anthropometric Measures and How Are They Assessed?
Anthropometric measures give a quick snapshot of status. Weight, height, and BMI classify risk: under 18.5 underweight, 18.5 to 24.9 normal, 25 to 29.9 overweight, 30 and up obese. Waist size and limb measures show changes in muscle and fat stores.
Skinfolds at the triceps, biceps, subscapular, or suprailiac site estimate body fat. Midarm muscle circumference is calculated as MAC minus 3.1414 times triceps skinfold in millimeters. In children, growth charts track trends over time.
Hydration affects these numbers. Edema or dehydration can skew weight and BMI. BMI also cannot separate muscle from fat, so it is one tool among many.
How Is Biochemical Data Collected and Analyzed?
Providers order blood and urine tests to reveal nutrition-related changes. Common tests include electrolytes, blood urea nitrogen, creatinine, glucose, cholesterol, triglycerides, liver enzymes, and a complete blood count.
Protein markers such as albumin, prealbumin, transferrin, and retinol-binding protein can reflect both nutrition and inflammation. Micronutrient panels check vitamins A, D, E, K, C, folate, and B12, plus minerals like iron, zinc, and selenium. C-reactive protein helps identify inflammation that can affect protein labs.
Results inform the plan: for example, low hemoglobin plus low iron stores suggests iron deficiency anemia. That calls for diet changes and possible supplements with follow-up testing.
What Nutrition-Focused Physical Signs Are Observed?
Physical signs add context you cannot get from labs alone. Clinicians note alertness, skin condition, and mobility. Body temperature, pulse, and blood pressure can point to infection, anemia, or metabolic strain.
Common clues include pale inner eyelids with iron deficiency, dry eyes with vitamin A shortage, or yellow eye whites with liver trouble. In the mouth, a swollen tongue, cracked corners, or bleeding gums can signal shortages of B vitamins or vitamin C.
Hair that is dry or breaks easily may reflect low intake of key nutrients. Nails that are brittle or spoon shaped can hint at protein or iron problems. Swelling in the legs may point to low protein status. Muscle wasting often appears with chronic illness and poor intake.
Simple changes can improve signs quickly. One client’s brittle hair improved within weeks after protein and micronutrient support, showing how fast targeted care can help.
How Do Socioeconomic and Lifestyle Factors Influence Nutrition Assessment?
Money, location, and culture shape what you eat. Limited income, disasters, or food deserts make it hard to buy fresh food. On the other hand, cheap processed foods can raise the risk for obesity.
Religious traditions and family habits change food choices and eating times. Alcohol or drug use can damage organs and block nutrient absorption. For women, cycle patterns matter. Heavy bleeding can drain iron. Oral contraceptives can lower some B vitamins and minerals.
In a free clinic, patients eating irregular meals due to unstable work often had peptic ulcer symptoms. Understanding these pressures made assessments more accurate and care plans more realistic.
Techniques and Tools for Nutrition Assessment
Think of these tools as your measurement toolkit. Each method captures a different part of the story.
How Is the 24-Hour Dietary Recall Used?
With a 24-hour recall, you list everything you ate and drank in the past day. You include portion sizes, cooking methods, and where you ate. The Automated Self-Administered 24-Hour Dietary Assessment Tool, or ASA24, is a free online option from the National Cancer Institute.
Clinicians review your responses for patterns and compare them to your needs. Many clinics also use apps for quicker entry and fewer mistakes.
What Are Food Frequency Questionnaires and How Are They Applied?
Food Frequency Questionnaires, or FFQs, ask how often you eat certain foods over weeks or months. Researchers use FFQs to study large groups because they are efficient and validated.
The NHANES FFQ focuses on frequency. The Diet History Questionnaire collects both frequency and portion size. You can find validated tools through Nutritools or the Validated Short Dietary Assessment Instruments database. Using a tested questionnaire improves accuracy and cuts guesswork.
How Is Body Composition Analysis Conducted?
Body composition methods separate fat mass and lean mass. Bioelectrical impedance analysis sends a safe, low current through the body to estimate these values, but hydration can change results. Dual-energy X-ray absorptiometry is a research standard, yet it costs more and uses a small amount of radiation.
Other methods include CT and MRI in special cases, often when imaging is done for another reason. Toolkits such as DAPA support standard measurement in clinics. Tracking lean mass helps set goals beyond weight alone.
What Biochemical Tests Are Performed in Nutrition Assessment?
Core tests include electrolytes, blood urea nitrogen, creatinine, glucose, lipid panels, liver enzymes, and a complete blood count. Protein markers, such as albumin and prealbumin, can help when interpreted alongside inflammation markers like C-reactive protein.
Micronutrient testing targets vitamins A, D, E, K, C, folate, and B12, plus minerals such as iron, zinc, and selenium. In select cases, absorption tests may be used for vitamin B12. These data points guide the care process from assessment to follow-up.
Advantages of Conducting Nutrition Assessments
Assessment turns scattered health information into a plan you can act on.
How Do Nutrition Assessments Enhance Health Outcomes?
Early detection leads to faster, safer care. Team-based screening and follow-up can cut infection rates, reduce hospital days, and lower the risk of serious complications. Hospitals that standardize screening often report lower costs and better results.
Routine monitoring also keeps your plan current. If lab values or weight trends change, your team adjusts the steps right away.
How Can Nutrition Assessments Prevent and Manage Chronic Conditions?
Assessments identify risks linked to diabetes, heart disease, and some cancers. Many people carry extra weight yet lack key nutrients such as vitamin D or iron. Addressing both problems together improves control and quality of life.
Ongoing checks track fasting glucose, A1C, lipids, and weight. Small, steady changes in your diet can meaningfully improve these numbers within weeks.
In What Ways Do Nutrition Assessments Boost Energy and Mental Clarity?
Low energy and brain fog often connect to nutrient gaps. Common culprits include low vitamin B12, iron, or vitamin D. Correcting these levels can lift concentration and stamina for work or school.
Balanced meals also stabilize blood sugar, which supports focus across the day.
How Do Nutrition Assessments Improve Athletic Performance?
Training raises your need for protein, carbohydrates, and micronutrients. Assessment checks if your intake meets those needs. Dietitians look for gaps that limit energy, slow recovery, or increase injury risk.
Plans based on assessment improve fueling and repair. In research, athletes following targeted plans recover faster and perform better (Thomas et al., 2016).
Target Audience for Nutrition Assessments
Everyone can benefit, yet some groups gain even more from structured screening.
Who Should Consider Nutrition Assessments When Managing Chronic Conditions?
Anyone managing diabetes, heart disease, cancer, or digestive disorders such as celiac disease or inflammatory bowel disease should consider regular assessment. People with dementia or absorption problems also benefit because they face higher deficiency risk.
In surgical care, patients with malnutrition often stay longer and face more infections. Assessment helps the team prepare a nutrition plan before and after surgery for safer recovery.
Why Are Pregnant and Breastfeeding Women Important Targets for Nutrition Assessments?
Pregnancy and breastfeeding increase needs for iron, folic acid, calcium, and vitamin D. Teens who are pregnant often need even more calcium to support bone growth. Assessments monitor these needs to protect you and your baby.
Past use of oral contraceptives and menstrual history can affect levels of B vitamins, vitamin C, magnesium, selenium, and zinc. Regular checks catch gaps early so care stays on track.
How Do Athletes and Physically Active Individuals Benefit from Nutrition Assessments?
Active people often need more iron, calcium, and protein. If you train hard, protein needs may reach 1.2 to 2 grams per kilogram of body weight daily. Assessment confirms whether your plan meets those targets.
Matching intake to training reduces fatigue and injury risk. It also speeds recovery between sessions.
What Are the Benefits of Nutrition Assessments for Aging Adults and Seniors?
Older adults face higher risk of malnutrition due to lower appetite, limited mobility, and reduced lean mass. Dental issues, chronic disease, and multiple medicines can also get in the way of eating well.
In hospitals, many older adults show signs of malnutrition. Regular screening identifies gaps in protein and micronutrients. This support helps maintain strength, independence, and quality of life.
How Do Nutrition Assessments Support Participants in Weight Management Programs?
Assessment distinguishes fat from lean mass, which is vital for safe weight change. BMI offers a starting point: under 18.5 underweight, 25 to 29.9 overweight, 30 and higher obesity. Body composition measures and waist size add detail beyond BMI.
Tracking over time prevents undernutrition and overnutrition. Your plan then adjusts to protect muscle and target fat loss.
Challenges in Effective Nutrition Assessments
Some barriers can blur the picture. Knowing them helps you plan better.
Why Is Self-Reported Dietary Data Often Unreliable?
Food records rely on memory and honesty. People forget snacks, misjudge portions, or change answers to appear healthier. This recall bias affects 24-hour recalls and FFQs.
Accuracy varies across ages and cultures. Studies comparing self-reports to objective measures, such as doubly labeled water, show frequent underreporting. Digital tools can improve accuracy with prompts and photo capture.
What Limits Accessibility to Advanced Testing Tools?
Cost and location limit access. DEXA scans, CT, and MRI are expensive and often not covered without a medical reason. Rural and low-resource clinics may only have scales, tape measures, and simple analyzers.
Hydration also affects some tests. For example, bioelectrical impedance can be off if you are dehydrated or have swelling.
How Can Cultural and Lifestyle Factors Affect Nutrition Assessments?
Cultural and religious practices guide food choices and eating times. Fasting periods or food restrictions change nutrient intake. Limited income pushes families toward cheaper, processed options, which can raise health risks.
Substance use and disordered eating further complicate reports. Clear, respectful questions and flexible plans help uncover the full picture.
Technological Advances in Nutrition Assessment
Digital tools make tracking and analysis easier to start and easier to sustain.
How Are Mobile Apps Used for Dietary Tracking?
Mobile apps let you log meals, snacks, and drinks in minutes. ASA24 offers a free online 24-hour recall supported by the National Cancer Institute. Nutritools provides guidance to pick validated methods that fit your goals.
Apps show calories and nutrients in real time and can send reminders. Barcode scanners speed entry. Regular tracking highlights patterns and nutrient gaps early.
| Mobile App | Key Features | Data Source |
|---|---|---|
| ASA24 | Guided 24-hour dietary recall, nutrient analysis | National Cancer Institute |
| Nutritools | Validated tool finder, best-practice guides | Nutrition research collaborations |
Built-in databases and dashboards improve accuracy and help you visualize progress over time.
What Role Do Wearable Devices Play in Monitoring Body Metrics?
Wearables track steps, heart rate, sleep, and estimated calories burned. These numbers provide objective context for your intake data. Many sync with apps to combine activity, sleep, and food logs.
Clinicians use this stream of data to fine tune energy targets and timing of meals around workouts or long shifts.
How Is AI Leveraged for Dietary Analysis?
AI-powered tools review what you log and flag trends such as low calcium or high added sugar. They suggest quick swaps, like choosing yogurt over a pastry, and update feedback as your habits change.
This speeds up analysis and reduces common logging errors, which supports better day to day choices.
The Role of Dietitian Nutritionists in Nutrition Assessments
Dietitian nutritionists turn raw numbers into practical steps you can follow.
How Do Dietitian Nutritionists Interpret Nutrition Data?
A registered dietitian nutritionist gathers your food history, lab results, body measurements, physical findings, and personal background. Using the Nutrition Care Process, the dietitian compares all data points to spot patterns and root causes.
For example, low hemoglobin with normal protein intake may point to poor iron absorption or ongoing blood loss. A dietetic technician may help with initial screening before you see the dietitian.
How Are Personalized Nutrition Plans Crafted?
Your plan is built from your intake, BMI or waist size, medical tests, and goals. A pregnant patient might focus on extra iron and folate. A person with diabetes may have specific carbohydrate targets and fiber goals.
Regular check-ins review food logs, labs, symptoms, and weight trends. Small adjustments keep the plan effective and realistic.
How Are Nutritional Interventions Adjusted Over Time?
Assessment is not a one time event. Follow-up visits measure weight change, lab values, grip strength, and daily function. These results guide next steps.
If your A1C improves after changing your breakfast and walking after dinner, the plan may shift to maintenance goals. If energy drops, your team revisits intake, sleep, and labs to find the cause.
Implementing Nutrition Assessments in Clinical Settings
Hospitals and clinics use nutrition assessments to guide treatment and track recovery.
How Do Nutrition Assessments Support Hospital and Healthcare Practices?
Standard screening catches risk early in high priority groups such as newborns, children, pregnant women, and older adults. Hospitals that screen and treat early often report fewer complications and shorter stays.
Routine screening builds a safer system. It helps teams decide when to bring in dietitians, start nutrition support, or order labs that confirm a suspected deficiency.
In What Ways Do Nutrition Assessments Aid Recovery and Rehabilitation?
Recovery after surgery, injury, or serious illness depends on adequate nutrition. Assessment identifies malnutrition, then guides protein and calorie targets for healing. This can cut infection rates and shorten time in the hospital.
Rehabilitation works best as a team effort. Dietitians manage intake and labs. Physicians, nurses, pharmacists, dentists, and lab staff solve related medical issues. With clear roles, nutrition becomes a central part of getting you back on your feet.
Conclusion
A complete nutrition assessment turns scattered clues into a plan you can use. It helps you detect malnutrition, manage chronic conditions, and improve energy, focus, and performance. With a registered dietitian guiding the nutrition care process, your plan adapts as your needs change.
This information is educational and is not a substitute for medical advice. Seek care right away for urgent symptoms, and work with your healthcare team to personalize any changes to your diet and supplements.
FAQs
1. What is nutrition assessment and why is it important for health?
Nutrition assessment uses scientific methods to evaluate a person’s dietary intake, physical measurements, and medical history. This process helps identify nutritional risks or deficiencies that may affect overall well-being. Research shows early detection through nutrition assessment can improve long-term health outcomes (Academy of Nutrition and Dietetics, 2020).
2. Which tools do experts use during a nutrition assessment?
Professionals often use food frequency questionnaires, 24-hour dietary recalls, anthropometric data such as height and weight, and laboratory tests like blood nutrient levels. These tools provide accurate insights into eating habits and nutritional status.
3. How does understanding your own nutrition help you make better choices?
Knowing your current diet patterns allows you to spot gaps in nutrients or excesses that could harm your health over time. For example, after my first detailed nutrition checkup with a registered dietitian last year, I learned my iron intake was low; this helped me adjust my meals to include more leafy greens and lean meats.
4. Who should consider getting a professional nutrition assessment?
Anyone interested in improving their wellness can benefit from an expert review of their eating habits; however people with chronic conditions like diabetes or heart disease gain the most value since tailored advice supports specific needs.
Summary: Nutrition assessments offer evidence-based guidance by using reliable tools to measure what we eat against our body’s needs; they empower individuals to make informed changes for lasting wellness benefits.







