Essential Chronic Kidney Disease Diet Food List For Healthy Eating
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
Looking for a clear Chronic Kidney Disease diet food list after your doctor raised concerns? Smart choices can protect kidney function and make daily meals easier to plan. With a kidney-friendly approach, you can manage sodium, potassium, phosphorus, and protein while still enjoying food.
This guide explains which fruits, vegetables, proteins, grains, fats, and drinks usually work well for people with CKD. You will also see what to limit, how to flavor food without salt, and where a dietitian fits in. Small, steady changes can support your kidneys and your energy.
Start with the basics and build meals that fit a renal diet.
Key Takeaways
- One in three adults with diabetes also has chronic kidney disease, so a kidney-friendly plan helps control blood pressure and mineral balance.
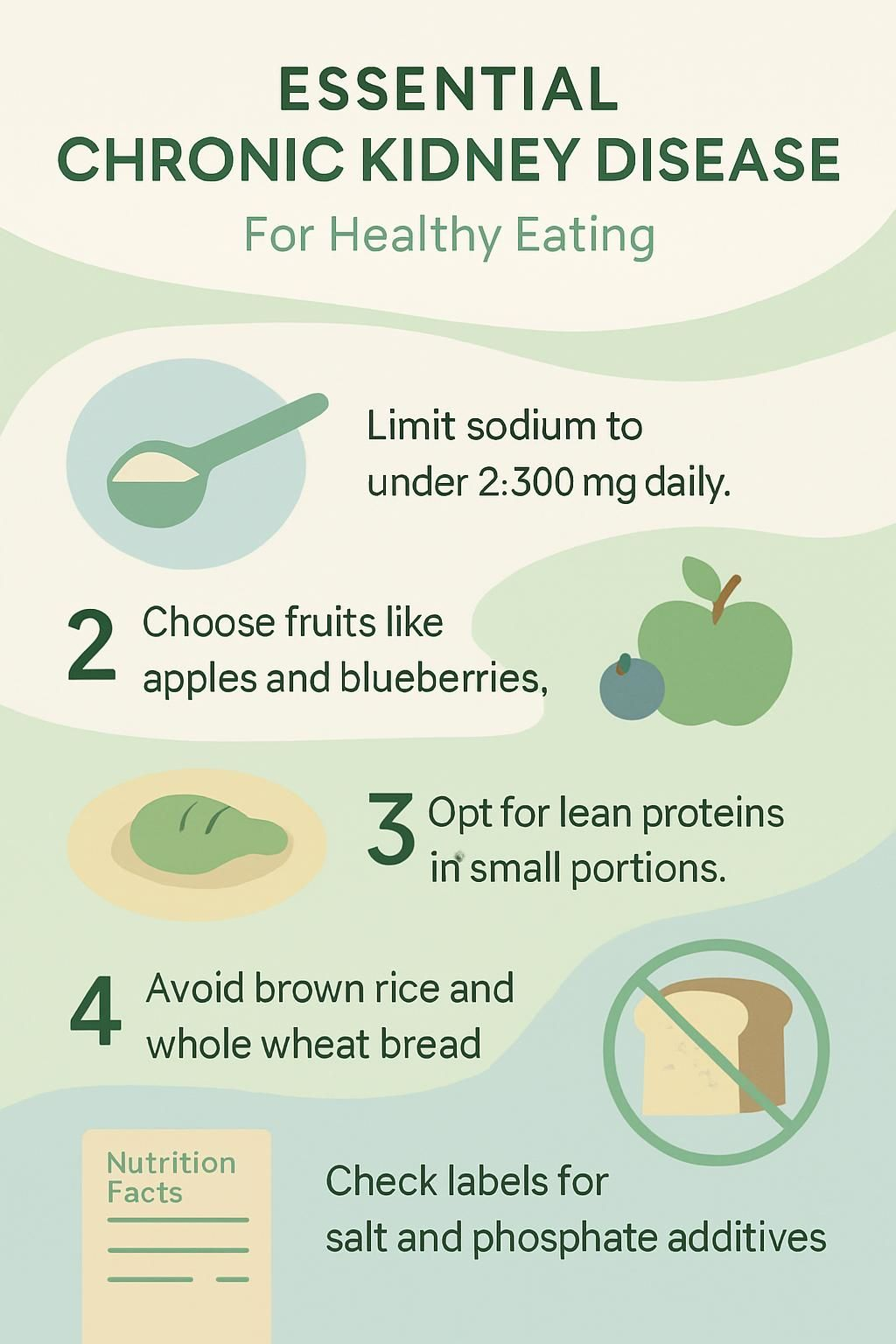
- Limit sodium to under 2,300 mg per day; pick items with 5 percent daily value or less per serving.
- Manage potassium and phosphorus: choose lower-potassium fruits like apples and blueberries, low-potassium vegetables such as cauliflower, and swap brown rice or whole wheat bread for lower-mineral grains.
- Use lean proteins such as skinless chicken, fish, egg whites, or tofu in measured portions; excess protein can strain kidneys unless you are on dialysis.
- Check labels for added salt and phosphate additives in processed foods; a registered dietitian can help you build a personal CKD meal plan.
Why a Kidney-Friendly Diet is Crucial for CKD Patients

Your kidneys filter blood, remove waste, and keep minerals like sodium, potassium, and phosphorus in balance. Chronic kidney disease reduces this work. Waste and extra fluid can build up, which may cause swelling in your legs and feet and leave you tired.
High levels of certain minerals raise the risk for high blood pressure, heart strain, weak bones, and muscle cramps. A kidney-friendly diet lowers that burden. Limiting sodium reduces fluid retention. Managing potassium helps prevent irregular heart rhythms. Controlling phosphorus supports bone health.
Many packaged foods hide sodium and phosphorus. Reading labels cuts these surprises at home and in the store. Fresh items usually give you more control over ingredients and portions.
You may notice that planning simple meals helps you avoid salty convenience foods and fast food. After two weeks of lower sodium, food often tastes fresher and herbs stand out.
Summary: Eat fresh more often, watch sodium, and limit high-potassium and high-phosphorus foods. These steps ease the workload on damaged kidneys. Sources include the National Kidney Foundation and the National Institutes of Health.
Key Nutrients to Manage in a Chronic Kidney Disease Diet
You will manage several key nutrients with CKD. Good control can slow kidney damage and support daily health.
How Much Sodium Should I Consume with CKD?
Kidneys with CKD do not handle sodium and water as well as healthy kidneys. Most experts, including the National Kidney Foundation, suggest less than 2,300 milligrams of sodium per day.
Check labels to track your total. Choose items that list 5 percent daily value or less of sodium per serving. Cook at home more often, and pick fresh produce, lower-sodium breads and grains, and unsalted snacks.
Lower sodium helps reduce blood pressure and swelling, which reduces strain on your heart and kidneys. Use herbs, garlic and onion powders, citrus juice, vinegars, pepper, and spice blends with no salt instead of table salt.
Avoid salt substitutes unless your doctor or dietitian approves them. Many contain potassium, which some people with CKD need to limit.
You may need about two weeks for your taste buds to adjust. Then food tastes brighter and less heavy.
These habits can slow damage from high blood pressure and make room for more whole foods in your plan.
How Can I Manage Potassium Levels in My Diet?
With kidney disease, clearing extra potassium can be hard. High potassium can affect heart rhythm. You may need to limit foods like oranges, potatoes, tomatoes, avocados, and whole-grain bread.
Examples: one medium banana has about 422 mg of potassium. One cup of tomato sauce has about 728 mg. A cup of prunes can reach 1,270 mg, and four dates have about 668 mg.
Swap to lower-potassium choices such as apples, berries, grapes, carrots, and cabbage. White bread usually has less potassium than whole wheat bread. If you enjoy potatoes, soaking or boiling them before cooking can cut potassium by up to 20 percent.
Some people need potassium binders, which are medicines that help remove potassium. Ask your doctor or dietitian about the right plan for your stage of CKD.
Why Is Controlling Phosphorus Important for Kidney Health?
Healthy kidneys remove extra phosphorus. With CKD, phosphorus can build up. High levels weaken bones and may cause itchiness and joint pain.
Foods high in phosphorus include meat, dairy, beans, nuts, whole wheat bread, brown rice, and many dark sodas. For reference, one cup of whole milk has about 205 mg, a slice of whole wheat bread has about 76 mg, and a cup of brown rice has about 149 mg. Dark sodas often include phosphorus additives, and your body absorbs additives more easily.
Cutting back helps protect bone and heart health. Your care team may also use phosphorus binders if diet changes are not enough.
Next, learn how much protein usually works with CKD.
What Is the Optimal Protein Intake for CKD Patients?
Protein needs balance. Too much protein can make kidneys work harder. Too little can lead to poor nutrition and weight loss. Good protein sources include egg whites, fish, tofu, and small portions of lean meat.
If you have stage 3 to 5 CKD and are not on dialysis, your dietitian may advise less protein. Dialysis patients often need more protein because treatments remove some. A dietitian can set targets based on labs and appetite.
Simple swaps help, such as using skinless chicken instead of red meat or tofu in place of beef in stir-fries. These changes reduce kidney stress and keep meals enjoyable.
How Do I Regulate Fluid Intake with CKD?
With advanced CKD, your doctor may limit fluids to reduce swelling and shortness of breath. Extra fluid can raise blood pressure and cause discomfort.
Track all drinks in a daily log. This makes small weight changes easier to spot before symptoms worsen. Water should be your main drink. Clear diet sodas, unsweetened tea, and small amounts of apple or grape juice can fit for variety. These choices are usually lower in potassium and phosphorus than orange juice or creamy coffee drinks.
Large servings of milk, creamers, syrups, or sugary drinks can raise minerals and calories. A diary app can help you see trends and stay within your limits.
Recommended Foods for a Chronic Kidney Disease Diet
Thoughtful choices can help protect your kidneys. Below are options that fit many CKD plans.
What Are the Best Fruits to Eat with CKD?
Fruits can satisfy cravings while keeping potassium in check. These are often safer picks.
- Apples are low in potassium and rich in fiber that helps you feel full.
- Blueberries are low in potassium and provide antioxidants that support general health.
- Grapes are low in sodium and potassium and offer hydration.
- Pineapple is a lower-potassium swap for oranges or bananas, about 180 mg per cup.
- Strawberries bring vitamins and fiber without heavy potassium.
- Cherries provide helpful plant compounds, choose fresh or frozen without syrup.
- Plums can fit in small portions, skip prunes due to higher potassium.
- Cranberries are a smart juice choice in small amounts if you need a low-potassium option.
Build snacks and desserts around these fruits to fit a renal diet. Balance portions, since serving size still matters.
Are Apples Good for Kidney Health?
Yes. A medium apple has about 158 mg of potassium, much less than oranges or bananas. Many kidney groups list apples as a go-to fruit for CKD.
Eat them whole, slice into salads, or add to oatmeal. Apples can also help steady hunger between meals. If you need a low-potassium juice for low blood sugar, apple juice is often used in small amounts.
Can Blueberries Help Manage CKD?
Blueberries are a smart pick for flavor and control. One cup has about 114 mg of potassium, which is low compared to many fruits. They also contain vitamin C and anthocyanins, plant pigments that support general wellness.
Add fresh or frozen berries to smoothies, yogurt alternatives, or salads. Keep portions moderate to stay within your daily goals.
Are Grapes Safe for a Kidney-Friendly Diet?
Grapes fit well for most people with CKD. One cup has about 288 mg of potassium. They are hydrating and easy to portion out.
Enjoy them as a snack, in salads, or chilled for dessert. If you manage diabetes too, grapes can fit into a balanced plan when you watch serving size.
Is Pineapple Suitable for CKD Patients?
Pineapple is a sweet, lower-potassium fruit choice. One cup has about 180 mg of potassium. It adds variety when you need to limit bananas or oranges.
Use fresh or frozen pineapple in fruit salads or low-sodium desserts. Portion control keeps minerals in a safe range.
Which Vegetables Support Kidney Health?
Many vegetables work well when you need to manage potassium and sodium. Fresh choices also help you avoid added salt.
- Cauliflower is low in potassium and sodium and provides vitamin C and fiber.
- Onions add flavor without salt and contain antioxidants that support blood vessels.
- Eggplant offers texture and is modest in potassium. Roast or bake it.
- Turnips are lower in potassium than potatoes. Mash or roast them for variety.
- Red bell peppers are colorful, low in potassium, and rich in vitamin C.
- Fresh vegetables are best. If you use canned, drain and rinse well.
- Boiling some vegetables can reduce potassium further, which helps with portion planning.
A quick tip: roasted red pepper sauce can replace tomato sauce in pasta dishes to lower potassium.
Is Cauliflower Good for CKD Diets?
Cauliflower is a strong choice. It is naturally low in potassium and phosphorus and works as a tasty swap for potatoes. Many CKD meal plans include it in place of higher-potassium sides.
Try it roasted, mashed, or riced. Pair with olive oil for healthy fat and flavor. Fresh cauliflower also helps you control sodium that often sneaks into boxed mixes.
Can I Eat Broccoli if I Have CKD?
Yes, in reasonable portions. Broccoli is modest in potassium and phosphorus and brings fiber and vitamins. Steaming or roasting are simple methods that preserve taste and texture.
Keep portions moderate so total potassium stays within your daily target.
Is Cabbage Beneficial for Kidney Disease?
Cabbage fits well in a renal diet. It is low in potassium and phosphorus and adds crunch and fiber. You can enjoy it raw in slaws, in soups, or in stir-fries.
High fiber also supports blood sugar control if you have diabetes with CKD. It is an easy way to add volume to meals without extra minerals.
Are Bell Peppers Recommended for CKD?
Yes. Bell peppers are low in potassium and phosphorus. A half-cup of chopped red pepper has about 88 mg of potassium and 10 mg of phosphorus.
Use them raw with dips or in stuffed pepper recipes that follow low-sodium rules. They add color, crunch, and vitamin C without heavy minerals.
What Protein Choices Are Best for Kidney Health?
Protein is essential, but portion control protects your kidneys. Choose lean and lower-phosphorus options most of the time.
- Lean poultry, such as skinless chicken or turkey, gives high-quality protein with less saturated fat. Avoid processed meats, which are high in sodium.
- Fish adds omega-3 fats that support heart health. Pick unsalted salmon, cod, or tilapia and aim for two servings per week.
- Egg whites provide protein with very little phosphorus or fat. Add to breakfast or mix into recipes.
- Tofu offers plant-based protein with modest phosphorus. Use it in stir-fries, soups, or salads.
- Lower-phosphorus cheeses, such as Swiss, Brie, goat cheese, mozzarella, parmesan, or Monterey Jack, can fit in small amounts.
- Keep portions modest. Aim for about 2 to 3 ounces of cooked meat or a half-cup of tofu per meal unless your care team advises otherwise.
- Needs change over time. Dialysis often raises protein requirements. Non-dialysis CKD often means limiting protein to protect remaining function.
- Mix animal and plant proteins to meet goals without excess mineral load.
Work with a renal dietitian to fine-tune portions based on your labs, appetite, and stage of CKD.
Is Skinless Chicken Safe for CKD?
Yes. Skinless chicken is a reliable lean protein for CKD. It tends to have less phosphorus and potassium than red meat, and it is easy to season without salt.
Choose unsalted cuts and keep serving sizes to 2 to 3 ounces cooked. Grill, roast, or bake to avoid extra fat.
Can I Eat Egg Whites with Kidney Disease?
Egg whites are usually a safe protein choice. Each large egg white has about 3 grams of protein and around 5 mg of phosphorus, much less than a whole egg.
Make omelets with egg whites and low-potassium vegetables. Watch total protein if you are not on dialysis, since too much can strain kidneys.
Is Fish a Good Protein Source for CKD?
Fish provides high-quality protein and healthy fats. It supports muscle and heart health, which is important with CKD. Avoid salty marinades and choose baking or grilling.
Portion control matters because protein and phosphorus still add up. Balance fish with low-potassium vegetables and lower-sodium grains.
Is Tofu Suitable for a Kidney-Friendly Diet?
Tofu works well in CKD plans. A half-cup has modest phosphorus and usually low sodium and potassium. It is a good swap when you want a plant-based option.
Use firm tofu in stir-fries or salads. Try silken tofu in smoothies or soups for a creamy texture without dairy.
Which Grains Are Beneficial for CKD?
Some grains carry less potassium and phosphorus. They can help you meet energy needs without extra mineral load.
- Choose white bread, buns, bagels, unsalted crackers, and pasta, which are often lower in potassium and phosphorus. A slice of white bread has about 32 mg of each.
- Pick bulgur, buckwheat, barley, or couscous instead of brown rice to cut phosphorus.
- Limit whole wheat bread if you need to manage potassium and phosphorus closely.
- Cook grains without salty broths or stock cubes.
- Use measured portions to meet energy goals without excess minerals.
- Consider enriched rice milk as a dairy alternative, which is often lower in phosphorus than cow’s milk or soy drinks.
- Check labels on crackers and packaged grain snacks for low sodium.
These swaps help you manage CKD and keep meals satisfying.
Is Quinoa a Good Grain Choice for Kidney Health?
Quinoa adds variety, fiber, and plant protein. It is not as high in potassium or phosphorus as many whole grains, but portions still matter.
Keep servings modest and pair quinoa with low-potassium vegetables like cabbage or bell peppers. This helps you stay within daily mineral targets.
Can Brown Rice Be Included in a CKD Diet?
Brown rice contains more potassium and phosphorus than white rice. One cup cooked has about 149 mg of phosphorus and 95 mg of potassium. White rice has about 69 mg of phosphorus and 54 mg of potassium per cup.
If you need strict limits, choose barley, buckwheat, bulgur, or couscous instead. Some people in early CKD can have small portions of brown rice, but check with your dietitian first.
Is Whole Wheat Bread Safe for CKD Patients?
Whole wheat bread offers fiber, but it is usually higher in potassium and phosphorus than white bread. A slice of whole wheat bread has about 76 mg of phosphorus and 90 mg of potassium, while white bread has about 32 mg of each.
For advanced CKD, many people do better with white bread. In early stages, small servings of whole wheat may fit with guidance. Sodium varies by brand, so compare labels.
What Healthy Fats Should I Include in My Diet?
Healthy fats support heart health and help you absorb vitamins. They also add flavor when you are cutting back on salt.
- Olive oil for cooking or salads. It is rich in monounsaturated fat and free of sodium.
- Safflower oil for baking or sautéing. It adds unsaturated fats without extra salt.
- Sesame oil in small amounts for flavor in stir-fries.
- Macadamia nuts in tiny portions, unsalted, for healthy fats and crunch.
- Unsalted, unsweetened nut butters in small amounts. Watch potassium content.
- Cream cheese or Brie in small servings if you need a softer cheese option.
- Canola oil as another heart-friendly choice that provides omega-3 fats.
Drizzle olive oil over steamed vegetables or use it in marinades with herbs and lemon. Simple swaps like these can help lower sodium while boosting taste.
Is Olive Oil Good for Kidney Health?
Yes. Olive oil contains mostly monounsaturated fat, which supports heart health without adding sodium or potassium. It is a top pick in many CKD plans.
Use it for sautéing low-potassium vegetables like broccoli and cauliflower or as a salad dressing base. It is also lower in phosphorus than many animal fats.
Are Macadamia Nuts Safe for CKD?
Macadamia nuts are lower in phosphorus and potassium than many other nuts. Choose unsalted versions and keep portions small to control calories and minerals.
Sprinkle a tablespoon over salads for crunch. This adds flavor without pushing your mineral targets too high.
Foods to Avoid or Reduce in a Kidney-Friendly Diet
Certain foods make mineral control much harder. Limiting them can improve blood pressure, fluid balance, and lab results.
Which High-Sodium Processed Foods Should I Limit?
Processed and restaurant foods often pack in salt. Cutting back helps protect your kidneys and heart.
- Processed meats such as hot dogs, bacon, sausage, pepperoni, and jerky. A 3-ounce serving can exceed 1,000 mg of sodium.
- Canned foods. Use low-sodium versions or drain and rinse to reduce salt.
- Packaged meals like frozen pizza, microwave dinners, and instant noodles. These can push you past 2,300 mg per day quickly.
- Pickles, olives, and relishes. One pickle spear has about 283 mg, five olives have about 211 mg, and two tablespoons of sweet relish have about 244 mg.
- Salty snacks, such as chips, pretzels, and many crackers.
- Restaurant meals, which often rely on added salt for flavor.
- Items listing more than 5 percent daily value of sodium per serving.
Switching from canned soup to homemade broth is one simple way to drop your sodium intake and support blood pressure control.
What Foods Are High in Phosphorus and Should Be Reduced?
If your kidneys do not clear phosphorus well, it builds up in the blood. Cutting back protects bones and the heart.
- Dark sodas with phosphorus additives, about 33.5 mg per 12 ounces.
- Dairy products like milk, yogurt, and many cheeses. One cup of whole milk has about 205 mg.
- Large servings of meat, beans, nuts, and seeds. Keep portions modest.
- Whole wheat bread and brown rice. One slice of whole wheat bread has about 76 mg, and a cup of brown rice has about 149 mg.
- High-phosphorus cheeses. Choose small portions or lower-phosphorus types.
- Canned and packaged snacks with phosphate additives. Check labels.
Reading labels for “phos” additives helps you avoid hidden sources that raise your intake.
How Can I Manage High-Potassium Foods in My Diet?
Many healthy foods are high in potassium. You may still enjoy some of them with careful portions and cooking methods.
Limit bananas, dried fruits, oranges, tomato products, potatoes, and many leafy greens if your labs run high. Choose lower-potassium options like apples, berries, cabbage, carrots, and grapes more often.
Use soaking and boiling methods for potatoes and some vegetables to reduce potassium. Your dietitian can set safe limits based on your stage of CKD and recent labs.
Preparing Meals for Chronic Kidney Disease
Meal prep helps you balance sodium, potassium, phosphorus, calcium, and protein. A renal dietitian can translate your goals into a weekly plan that fits your life.
How Can I Flavor Food Without Adding Sodium?
Season food with fresh herbs, spices, and acid. Garlic and onion powder add flavor without salt. Lemon or lime juice, vinegars, mustard, pepper, and salt-free blends brighten dishes.
Cooking at home usually cuts sodium compared with packaged items and takeout. Your taste adjusts within 1 to 2 weeks, making natural flavors shine.
Ask your dietitian which seasoning blends are low in potassium and phosphorus and right for your plan.
Why Should I Prioritize Fresh Ingredients for CKD Meals?
Fresh ingredients help you control sodium, potassium, and phosphorus. Many processed foods include additives that raise these minerals without clear warning.
Choose fresh meats or fish instead of cured or deli options. Pick fruits and vegetables that match your potassium goals. Apples, berries, cabbage, and peppers are often safer than oranges or tomato-heavy dishes.
Home cooking lets you use herbs and citrus for flavor, not salt. It also makes portion tracking easier.
How Do I Monitor Portion Sizes for Kidney Health?
Measure with cups, spoons, or a food scale. Smaller plates can help you serve less without feeling deprived.
Limit whole wheat bread and brown rice if you need to reduce phosphorus and potassium. Watch processed meats, pickles, olives, and dairy due to sodium and phosphorus.
Work with a dietitian to fine-tune portions. Careful tracking helps prevent mineral buildup that can stress kidneys.
How a Dietitian Helps in CKD Diet Management
A renal dietitian gives you a plan that fits your stage of CKD, lab results, and preferences. You may target under 2,300 mg of sodium per day and limit potassium and phosphorus as needed.
Your dietitian can teach methods such as soaking and boiling to lower potassium in certain vegetables. Regular check-ins help adjust your plan if your labs change or if you start dialysis.
Many people find label reading much easier after one focused session. This support turns goals into clear daily steps.
Conclusion
Choosing kidney-friendly foods can help you manage chronic kidney disease. Build meals around fruits and vegetables that fit your potassium target, lower-mineral grains, lean protein, and healthy fats like olive oil. Keep sodium under 2,300 mg per day to protect your heart and kidneys.
Read labels for added salt and phosphorus additives. Cook fresh meals more often, and flavor food with herbs, citrus, and spices instead of salt. A registered dietitian can help you shape a personal kidney diet that fits your lifestyle and stage of CKD.
This article is for education only. It does not replace advice from your doctor or dietitian. If you have symptoms such as swelling, shortness of breath, or rising lab values, contact your care team promptly.
FAQs
1. Which foods are high in potassium and should people with chronic kidney disease limit?
Bananas, oranges, potatoes, tomatoes, spinach, and avocados are foods that are high in potassium. People with chronic kidney disease often need to limit these foods because their kidneys may not remove extra potassium well. High blood potassium can cause heart problems according to the National Kidney Foundation.
2. Why is it important for those with chronic kidney disease to watch their intake of foods high in potassium?
People with chronic kidney disease have reduced ability to filter out excess minerals like potassium from the blood. Eating too many foods that are high in potassium can lead to dangerous levels which may affect heart rhythm or muscle function as shown by clinical studies.
3. What alternatives exist for common foods that are high in potassium on a healthy eating plan for chronic kidney disease?
Apples, berries, grapes, cauliflower, rice cereal, and white bread contain less potassium than bananas or potatoes. Swapping these lower-potassium options helps keep blood mineral levels safer while still providing variety and nutrition.
4. How do I know if my diet contains too many foods that are high in potassium when managing chronic kidney disease?
A registered dietitian can review your food list and check your lab results for signs of elevated blood potassium levels. In my own experience working with patients at a local clinic who tracked their meals closely using food diaries saw better control over their health outcomes after adjusting how often they ate certain fruits and vegetables.
Summary: Foods such as bananas and tomatoes rank among those highest in dietary potassium content; limiting them supports healthier living for individuals diagnosed with chronic kidney issues according to evidence-based guidelines from nephrology experts.







