Diet For Kidney Disease: A Renal-Friendly Guide For Chronic Kidney Disease Patients
Our Nutrition Assistant AI Suite will transform your body. You will lose fat, get toned, and build muscle. Gain confidence and optimal health.
Many people with chronic kidney disease wonder which foods protect their kidneys and which foods cause stress. I felt the same confusion at first. A clear renal diet, also called a kidney diet, makes daily choices easier and supports kidney function.
After learning this, I spent time reviewing research and working with my care team. This guide shares the basics of healthy eating for people with kidney disease, including limits for key minerals and simple meal planning tips you can use today.
Small steps matter. With a few mindful swaps, you can ease symptoms, support your heart, and feel better each day. This article is educational, not medical advice. Talk with your healthcare team before changing your plan.
Key Takeaways
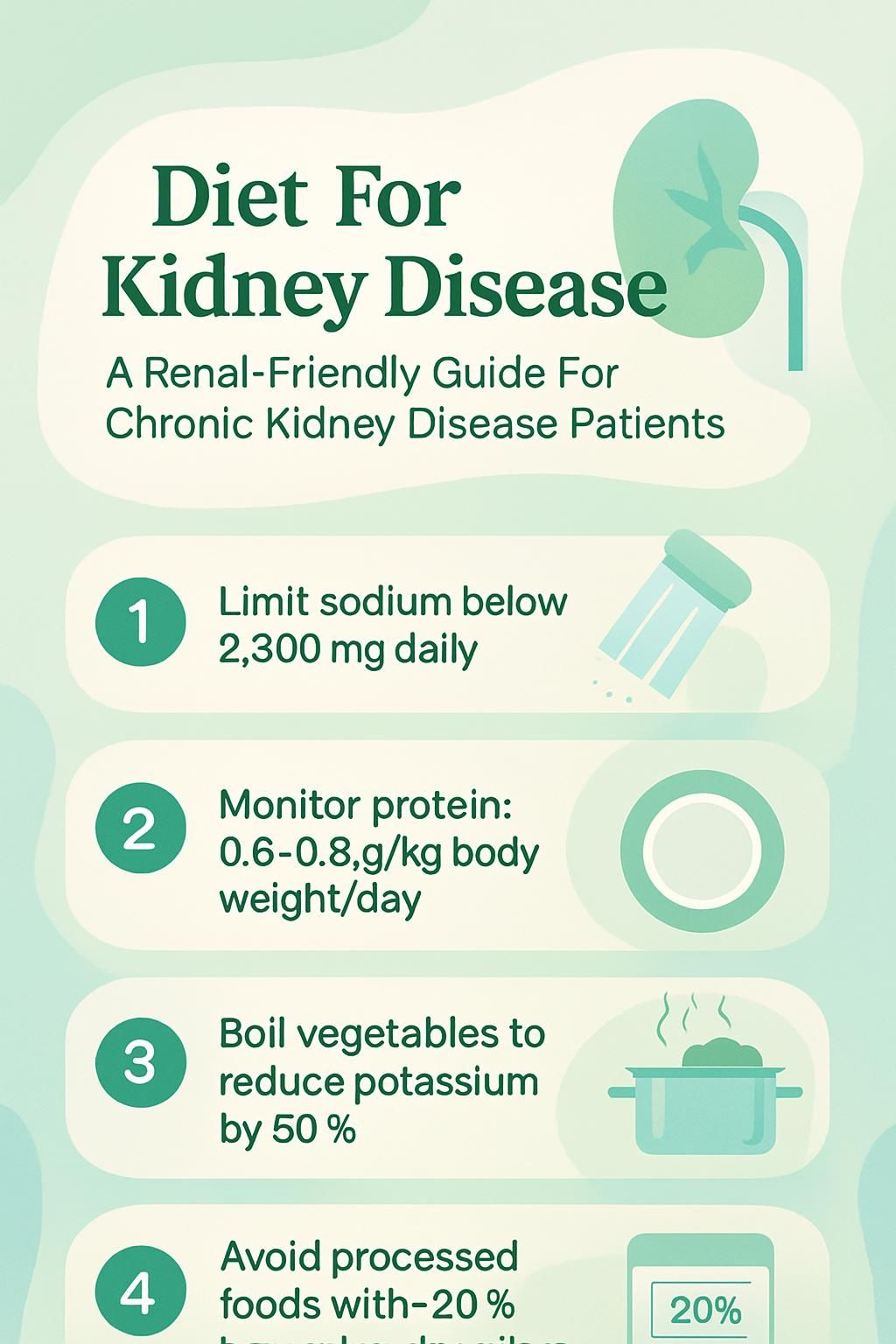
- Limit sodium to under 2,300 mg per day; manage potassium and phosphorus to lower risks for high blood pressure, heart problems, and bone issues.
- Before dialysis, many adults aim for about 0.6 to 0.8 grams of protein per kilogram of body weight each day to reduce waste the kidneys must filter.
- Avoid processed foods with high sodium, salt substitutes with potassium chloride, and phosphate additives labeled with “PHOS.”
- Boiling and then draining vegetables can cut potassium by up to 50 percent, a method supported by National Kidney Foundation guidance.
- Work with a registered dietitian to match your renal diet to your CKD stage. Medicare covers Medical Nutrition Therapy in the United States with a doctor’s referral.
Why Is a Kidney-Friendly Diet Important?

A renal diet reduces extra fluid and waste that damaged kidneys struggle to remove. Careful food choices can slow loss of kidney function and improve daily life.
How does diet affect chronic kidney disease?
Diet shapes how hard the kidneys must work. Sodium, potassium, and phosphorus are minerals that can build up in the blood when kidneys do not filter well.
High sodium pulls in water and raises blood pressure, which strains the kidneys and heart. Too much phosphorus weakens bones and can cause itchiness or joint pain. High potassium can trigger unsafe heart rhythms in advanced CKD.
Balanced nutrition lowers this burden and may slow CKD progression. The National Kidney Foundation notes that smart diet changes reduce risks for swelling, bone disease, and cardiovascular problems. Many people also limit protein because extra protein creates more waste that injured kidneys cannot clear well.
“What you eat has a real effect on how your kidneys work each day.”
What are the benefits of a renal-friendly eating plan?
I noticed less swelling and steadier blood pressure after cutting sodium. Keeping potassium and phosphorus in range helped my energy and sleep. The National Institute of Diabetes and Digestive and Kidney Diseases reports that these changes support fluid balance and heart health.
Plant-forward meals, healthy fats like olive oil, and simple cooking methods help reduce complications over time. Working with a registered dietitian gave me a clear plan and realistic goals, including delaying dialysis as long as safely possible.
Key Nutrients to Monitor in a Renal Diet
Managing a few key nutrients protects kidney health. I focus on sodium, potassium, phosphorus, protein, fluids, and calories, then adjust based on my labs and CKD stage.
Why limit sodium intake in kidney disease?
Too much sodium leads to fluid retention and higher blood pressure, which can damage kidneys further. People with CKD often need stricter limits than the general 2,300 mg per day target.
Sodium hides in many processed foods, including canned soup, frozen meals, chips, crackers, cured meats, cheese spreads, and condiments. I use Nutrition Facts labels to spot high sodium products. A 20 percent Daily Value or more is high; 5 percent or less is low.
Reducing sodium helps control swelling and reduces strain on failing kidneys.
How does potassium affect kidney health?
Healthy kidneys balance potassium. With CKD, potassium can rise, which may cause muscle weakness or dangerous heart rhythms. Clinicians monitor potassium with regular blood tests and adjust the diet as needed.
High-potassium foods include bananas, avocados, oranges, potatoes, beans, dried fruit, and tomato sauce. Some salt substitutes use potassium chloride, which can be unsafe if you must limit potassium.
Cooking tips help. Boiling potatoes or other vegetables lowers potassium. Draining and rinsing canned fruits or vegetables also reduces it. My team tailors my target based on my stage and labs, and potassium binders may be used if diet alone is not enough.
What is the role of phosphorus in a renal diet?
Phosphorus is important for bones and cells, but high levels harm blood vessels and bones in CKD. Symptoms can include itch, bone pain, and brittle bones.
Many protein foods contain phosphorus, including meat, dairy, beans, and some grains. Added phosphates appear on labels with “PHOS” in the ingredient list and absorb quickly. My dietitian taught me that animal phosphorus absorbs more easily than plant phosphorus from beans and nuts. Blood tests guide whether I need a phosphate binder.
Fruits and many vegetables are lower in phosphorus, especially compared with processed foods. I check labels and choose fresh foods when possible.
How much protein should CKD patients eat?
Protein supports muscles and healing, yet too much creates extra waste. Many adults with CKD who are not on dialysis aim for about 0.6 to 0.8 grams of protein per kilogram of body weight daily. Your clinician may adjust this range.
Dialysis removes some protein, so people on dialysis usually need more. Lean poultry, eggs, fish, and tofu offer quality options. Plant proteins tend to bring less absorbed phosphorus, which can help keep blood levels in range.
How do fluids impact kidney disease management?
Fluids affect swelling, blood pressure, and breathing comfort. Early CKD may not require fluid limits. Later stages often do, especially if swelling or rapid weight gain appears.
I count all liquids, including water, coffee, tea, milk, soup, gelatin, and ice cream. Not enough fluid can cause low blood pressure and dizziness. Too much can cause swelling and shortness of breath. My provider adjusts targets as my condition changes.
Why are calories important in a kidney-friendly diet?
Getting enough calories prevents weight loss and muscle loss. Low calorie intake raises the risk of malnutrition and a weaker immune system, especially if appetite or taste changes.
A dietitian can suggest foods that deliver energy without too much sodium, potassium, or phosphorus. I use safe carbs like bread or rice, add healthy fats like olive oil, and select proteins that match my goals. This keeps my energy steady and my labs stable.
Next, I cover specific foods that fit well in a kidney-friendly meal plan.
What Foods Should You Include in a Kidney-Friendly Diet?
I pick foods that nourish me without overloading my kidneys. Variety helps me meet goals and enjoy meals.
Which low-potassium fruits and vegetables are best?
Low-potassium produce helps keep blood levels safe while adding fiber and flavor.
- Peaches, grapes, and pineapple are usually safer than bananas or oranges for most people with CKD.
- Cabbage is low in potassium and high in vitamin C. I add it to salads or soups.
- Carrots add fiber and color without a large potassium load per serving.
- Cucumbers are refreshing, low in potassium, and easy to slice for snacks.
- Drain and rinse canned fruits and vegetables to lower potassium picked up during processing.
- Boiling vegetables like carrots or cabbage, then draining, can lower potassium before eating.
- Needs vary by stage. Rotate choices to meet your plan and prevent boredom.
What are good lean protein options for CKD?
Picking the right proteins limits phosphorus and saturated fat while meeting daily needs.
- Skinless turkey or chicken without phosphate additives gives high-quality protein with less fat.
- Egg whites supply protein with very little phosphorus and no cholesterol.
- Plant proteins like beans and tofu often have less absorbed phosphorus than meats.
- Fish such as cod, tilapia, or tuna provide lean protein and less saturated fat than many red meats.
- Lean beef or pork labeled “loin” or “round” can fit in small portions if your team approves. Skip processed versions with extra sodium and phosphates.
- Plain Greek yogurt may fit in small amounts if your plan allows dairy. Ask your dietitian.
- Protein targets change with CKD stage. A registered dietitian can set the safest range for you.
These options support muscles while keeping phosphorus and sodium in check.
How do whole grain carbohydrates support kidney health?
Whole grains offer steady energy and fiber, which support heart and kidney health, especially if you also manage diabetes.
- Brown rice, multigrain hot cereal, and whole-wheat soda bread provide complex carbs for stable blood sugar.
- Fiber supports digestion and may lower cholesterol, which protects the heart and kidneys.
- Many whole grains are naturally low in sodium and phosphorus compared with instant products.
- Energy from whole grains helps reduce fatigue during daily tasks.
- Research shows eating several servings of whole grains each day supports energy without overloading minerals in many people.
- Plant-forward patterns may also reduce acid build-up, which can support kidney function over time.
- I use whole-wheat bread or cereal as a base, then add low-potassium produce for balance.
Which healthy fats are safe for kidney disease patients?
Healthy fats support heart health and help absorb fat-soluble vitamins. I pick unsaturated fats and watch portions.
- Canola and safflower oils provide unsaturated fats without extra sodium.
- Avocado is rich in healthy fat and low in sodium, though I keep portions small due to potassium.
- Nuts and seeds add healthy oils and fiber. Portions may be larger for people on dialysis who need more calories.
- Olive oil replaces butter in many recipes to lower saturated fat intake.
- Fatty fish like salmon or trout provide omega-3 fats that support heart health.
- Limit solid fats from red meat, poultry skin, and butter to manage cholesterol and heart risk.
- Olive or rapeseed oil sprays help cook with less fat and less sodium.
Next, I focus on foods to limit, which can quietly raise sodium, potassium, or phosphorus.
What Foods Should You Avoid on a Renal Diet?
Some foods strain the kidneys or push minerals out of range. Keeping an eye on labels helps me stay safe.
Why avoid high-sodium processed foods?
High-sodium foods cause fluid retention and make the heart and kidneys work harder. Big sources include canned foods, frozen dinners, processed meats, chips, crackers, and salty sauces like soy sauce or ketchup.
The Dietary Guidelines for Americans suggest 2,300 mg sodium per day for most adults, but many people with CKD need less. Reading labels helped me lower sodium gradually and retrain my taste buds. Cooking at home with fresh ingredients made the biggest difference.
Which high-potassium foods should be limited?
Oranges, bananas, tomatoes, and potatoes often raise potassium quickly. Many salt substitutes use potassium chloride, which can be unsafe if you have a potassium limit.
I check labels for potassium chloride in snacks or canned goods. Boiling vegetables, draining canned produce, and choosing juices like apple, grape, or cranberry instead of orange help me manage potassium. These steps keep my labs steady.
What foods high in phosphorus should CKD patients skip?
Dairy foods like cheese, milk, and yogurt contain phosphorus. Beans, nuts, and seeds are also high. Many packaged foods add phosphates, which show up on labels with “PHOS.”
Deli meats and certain flavored drinks may contain added phosphates that absorb easily. Meats, especially organ meats, often deliver more absorbed phosphorus than plant foods. If blood tests stay high, clinicians may prescribe phosphate binders. I lean on fruits and lower-phosphorus vegetables to keep variety without pushing my levels up.
Why avoid salt substitutes with potassium chloride?
Many reduced-sodium seasonings contain potassium chloride. Weakened kidneys cannot remove extra potassium well, which can raise the risk of abnormal heart rhythms and muscle weakness.
Once I learned my lite salt was spiking my potassium, I switched to herbs, spices, citrus, and vinegar for flavor. Reading ingredient lists prevents surprises.
How Can You Create a Personalized Renal Diet?
I work with my dietitian to adjust targets as my labs and symptoms change. A personal plan makes daily choices clearer and safer.
Why work with a registered dietitian?
A registered dietitian translates lab results into practical meals. In early stages, we might focus on sodium and protein. Later, we may tighten potassium or phosphorus and watch fluids closely.
If appetite drops or food tastes change, a dietitian helps me maintain calories and protein. Medicare covers Medical Nutrition Therapy in the United States with a doctor’s referral. Expert guidance keeps me on track when my needs shift.
How does your CKD stage affect your diet?
Nutrition needs change as CKD progresses. Early on, many people have fewer limits. In advanced stages, I manage fluids, limit sodium more tightly, and track minerals closely.
Dialysis increases protein needs because treatment removes some protein. My plan changes with each set of labs, which helps prevent complications like high potassium or high phosphorus. The goal stays steady, slow disease progression and protect health with balanced nutrition.
How to adjust portion sizes and cooking methods?
Portions and cooking styles can lower nutrient overload without losing flavor. Small changes add up.
- I measure portions with a cup or scale to avoid excess calories, protein, sodium, or phosphorus.
- Cooking from scratch gives me control over sodium and additives that processed foods often hide.
- Boiling vegetables and draining the water helps cut potassium by as much as 50 percent in some vegetables.
- I remove poultry skin and trim visible fat to lower saturated fat.
- I replace butter with olive oil or a nonstick spray for a lighter finish.
- I use grilling, air-frying, baking, roasting, broiling, or stir-frying instead of deep-frying.
- I shrink portions gradually so changes feel realistic and last.
- I read labels for sodium and phosphorus to meet daily limits.
- I pick lean proteins like fish or egg whites to meet protein needs safely.
These steps keep meals satisfying while protecting my kidneys.
Why is reading food labels important?
Labels show serving size and percent Daily Value for sodium and other nutrients. Five percent DV or less is low; 20 percent or more is high. This quick check helps me compare products fast.
Ingredient lists reveal added phosphates with “PHOS.” Claims like sodium-free, very low sodium, reduced sodium, no salt added, or unsalted guide my choices. Careful label reading cuts hidden mineral intake from packaged foods.
What Are the Best Cooking Methods for CKD Patients?
Simple techniques can lower sodium and potassium while keeping flavor. I rely on methods that need little added fat or salt.
How does boiling help reduce kidney strain?
Boiling pulls potassium out of vegetables and into the water. Cutting food into smaller pieces increases this effect.
I drain and discard the cooking water to reduce potassium. Rinsing canned vegetables and then heating them in fresh water can also lower sodium. Many clinicians recommend boiling for people who must control potassium tightly.
Why is steaming a good cooking method for CKD?
Steaming preserves texture and nutrients without much fat or sodium. It helps me avoid heavy oils and salty seasonings.
I steam vegetables in batches for quick meals later. This supports heart health and fits kidney diet goals. Many steamed vegetables also end up lower in potassium than raw portions after cooking and draining.
When should baking be used for renal-friendly meals?
Baking is great for lean proteins like fish or chicken and for whole grain sides. It keeps flavors strong without lots of salt or added phosphorus.
Batch cooking helps with portion control and saves time. I roast vegetables with olive oil and herbs for a simple, kidney-friendly side with bright flavor.
How does grilling fit into a kidney-friendly diet?
Grilling adds smoky flavor without heavy sauces. Extra fat drips off, which lowers saturated fat in meats.
I grill kebabs with peppers and onions or pineapple slices and season with herbs, citrus, or vinegar instead of salty marinades. This makes it easier to keep sodium under 2,300 mg per day and still enjoy meals.
How Do You Manage Special Dietary Needs with CKD?
Many of us manage CKD alongside other conditions. Planning helps you meet both sets of needs safely.
How to adjust a renal diet for diabetes?
I pair carbs with lean protein or healthy fat to steady blood sugar. Whole grains, lower-potassium fruits, and suitable vegetables help me control glucose and support kidney health.
If I need quick treatment for low blood sugar, I choose apple, grape, or cranberry juice instead of orange juice. My dietitian fine-tunes the plan and may suggest medication changes if needed.
Clear labels and careful sodium limits reduce thirst and help with fluid control. That matters more as CKD advances.
What are fluid restriction guidelines for advanced CKD?
In advanced CKD, clinicians may set a daily fluid limit to prevent swelling and shortness of breath. Fluids include drinks, soups, gelatin, ice cream, and watery fruits.
Many people stay between 32 and 48 ounces a day, based on labs and symptoms. Missing dialysis can allow fluid to build up quickly. If I notice swelling or fast weight gain, I contact my care team for guidance.
Protein targets also matter. Your team will tailor both fluid and protein goals to your stage and symptoms.
What Is the Role of Medical Nutrition Therapy (MNT) in CKD?
Medical Nutrition Therapy is nutrition counseling from a registered dietitian. It matches your diet to your stage of CKD and your lab results.
How does MNT benefit CKD patients?
MNT can slow CKD progression and improve quality of life. Dietitians set targets for sodium, potassium, phosphorus, protein, and calories. They also help prevent malnutrition.
In my case, MNT clarified how much protein I need and which foods fit my plan. Studies link MNT with better control of mineral levels and fewer heart-related risks in CKD.
Is MNT covered by insurance?
Medicare covers MNT for CKD when ordered by a physician and provided by a registered dietitian. Private coverage varies, so I called my insurer to confirm visit limits and costs.
If coverage is limited, ask about community programs or low-cost clinics. Consistent follow-ups help me meet nutrition goals as my labs change.
Next, I prepare questions for my healthcare team so we can adjust my meal plan with confidence.
What Questions Should You Ask Your Healthcare Team?
I bring a short list to each visit. Clear questions help me align my diet with my labs and symptoms.
How can I balance nutrients in my diet?
I track sodium, potassium, phosphorus, protein, and calories using Nutrition Facts labels and a simple log. Blood tests guide changes. Healthy fats and smart portions support my heart.
A registered dietitian matches targets to my CKD stage and helps me avoid malnutrition. This stepwise approach keeps my plan safe and realistic.
Are there specific foods I should avoid?
I limit processed and restaurant foods, which are usually high in sodium. I also avoid processed meats like bacon, sausage, and cured deli cuts that bring a lot of salt and additives.
High-phosphorus choices, such as dairy, beans, nuts, seeds, bran cereals, dark colas, and chocolate drinks, may need limits. Many people also restrict high-potassium fruits like oranges or bananas. I skip salt substitutes with potassium chloride to prevent heart rhythm issues.
My care team personalizes this list based on my labs and stage.
How do I manage fluid intake effectively?
I count all liquids toward my daily limit, including soups and frozen treats. If I swell or gain weight fast, I call my clinician because that may signal fluid overload.
Keeping sodium low reduces thirst and helps with fluid goals. Fresh foods, herbs, and acid from lemon or vinegar make meals tasty without adding salt.
What Resources Are Available for CKD Patients?
Helpful tools make planning easier. I use trusted sources to guide shopping and cooking and to track my progress.
Where can I find meal planning tools?
I use resources from the U.S. Department of Agriculture for balanced meal ideas. My dietitian provides worksheets and apps for tracking fluids and nutrients. The National Kidney Foundation shares stage-based tips and recipes.
My kidney specialist also points me to local services that improve access to healthy foods. I like simple trackers for protein grams, sodium under 2,300 mg per day, and produce choices that match my stage.
What are some kidney-friendly recipes?
Low-sodium, lower-potassium, and lower-phosphorus recipes protect the kidneys while keeping meals enjoyable. I make avocado deviled eggs in small portions, vegetable dips with minimal salt, and grilled pineapple for a bright side.
For drinks, blackberry iced tea or blueberry lemonade keeps sodium and sugar modest. I rotate vegetable stir-fry, baked fish, or chicken salad with a light vinaigrette. A baked blueberry French toast on weekends feels special yet fits my plan.
For more guidance, the Mayo Clinic and similar organizations offer recipes and meal ideas aligned with CKD nutrition principles.
How can support groups and educational materials help?
Support groups connect me with people who understand the daily challenges. Sharing tips helps me stay consistent.
Educational guides from trusted groups explain sodium, potassium, phosphorus, protein, and calories in plain language. Clear information helps me adjust my diet with confidence at each stage.
Conclusion
Careful food choices can protect kidney function and lower symptoms of chronic kidney disease. Keeping sodium, potassium, and phosphorus in range, choosing the right amount of protein, and watching fluids all support a stable plan.
Working with a registered dietitian turns goals into a daily eating plan you can follow. With steady habits and credible resources, you can support your kidneys, your heart, and your quality of life. This guide is for education only. Always follow advice from your healthcare team for your specific stage of CKD.
FAQs
1. What is a renal-friendly diet for chronic kidney disease patients?
A renal-friendly diet focuses on nutrition that supports kidney health. It limits sodium, potassium, and phosphorus intake while ensuring enough protein and calories to meet the body’s needs. This approach helps slow the progression of chronic kidney disease.
2. Are nuts (fruit) safe for people with kidney disease?
Nuts are high in nutrients but can contain significant amounts of potassium and phosphorus. Patients with chronic kidney disease should check serving sizes and consult their healthcare provider before adding nuts to their diet.
3. How does proper nutrition help manage chronic kidney disease?
Proper nutrition helps control blood pressure, reduces waste buildup in the body, and maintains healthy levels of minerals like sodium and potassium. Studies show that following a tailored meal plan improves quality of life for those living with chronic kidney problems.
4. Can you share an example of applying these dietary guidelines in daily life?
After my diagnosis, I worked closely with a registered dietitian who helped me read food labels carefully and choose snacks low in salt or added sugars instead of processed foods or certain nuts (fruit). Over time, this made it easier to keep my lab results stable.
Summary: A well-planned diet rich in appropriate nutrients plays a key role in managing chronic kidney disease; careful selection of foods such as nuts (fruit), guided by professional advice, supports better health outcomes for patients.







